Expanding the Therapeutic Reach of Chimeric Antigen Receptor T-Cells and Bispecific T-Cell Engagers Across Solid TumorsGerber, Xie, Patel
JCO Precis Oncol (2025) 9, e2400753
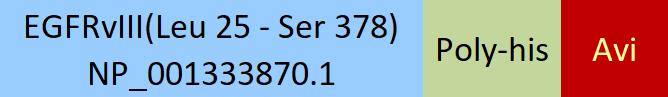
Abstract: The introduction of T-cell-based therapeutics in hematologic malignancies has led to improvements in outcomes for patients with acute leukemia, lymphoma, and multiple myeloma. To date, the Food and Drug Administration (FDA) has approved seven chimeric antigen receptor-T (CAR-T) cell therapies and seven bispecific T-cell engagers (BiTEs) across a variety of hematologic malignancies; however, the extension of CAR-T therapies and BiTEs to the solid tumor arena has been somewhat limited. In this review, we discuss the landmark data that led to the commercialization of four novel FDA-approved T-cell-based therapeutics in solid malignancies, including tarlatamab for small cell lung cancer, afamitresgene autoleucel for synovial sarcoma, lifileucel for metastatic melanoma, and tebentafusp for metastatic uveal melanoma. We discuss the targetable antigen landscape of CAR-T therapies and BiTEs under investigation in solid malignancies. We explore the translational potential for various CARs under active investigation, including human epidermal growth factor receptor 2-directed CARs in breast cancer, prostate stem cell antigen-directed CARs for prostate cancer, epidermal growth factor receptor (EGFR)-IL13Ra2 and EGFR-vIII CARs for glioblastoma, and GD2-directed CARs for neuroblastoma. We glean from lessons learned for existing CAR-T therapies and BiTEs for hematologic malignancies and emphasize solutions toward facilitating the clinical rollout of T-cell-based therapies in solid tumors, including scalability to meet the growing needs of clinical oncology. Some solutions include addressing on-target, off-tumor toxicity; improving the manufacturing of CARs; optimizing the tissue-specific tumor microenvironment by combating immune desert tumors; and discovering natural tumor neoantigens and non-self-epitopes generated by tumor-specific mutations. These concepts can help provide transformative benefits for patients with solid malignancies in the coming years.
Engineering Multifunctional Peptide-Decorated Nanofibers for Targeted Delivery of Temozolomide across the Blood-Brain BarrierBellavita, Barra, Braccia
et alMol Pharm (2025)
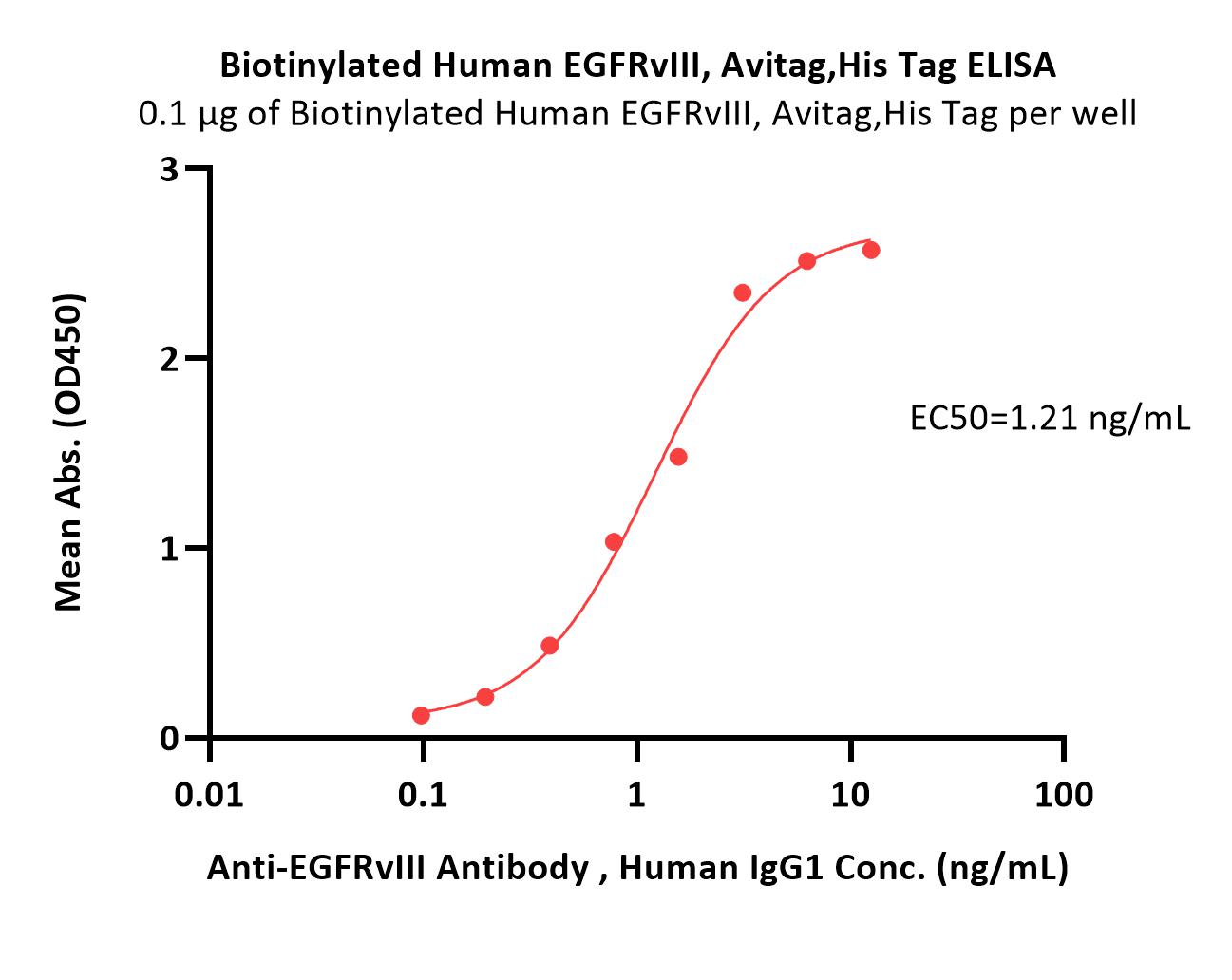
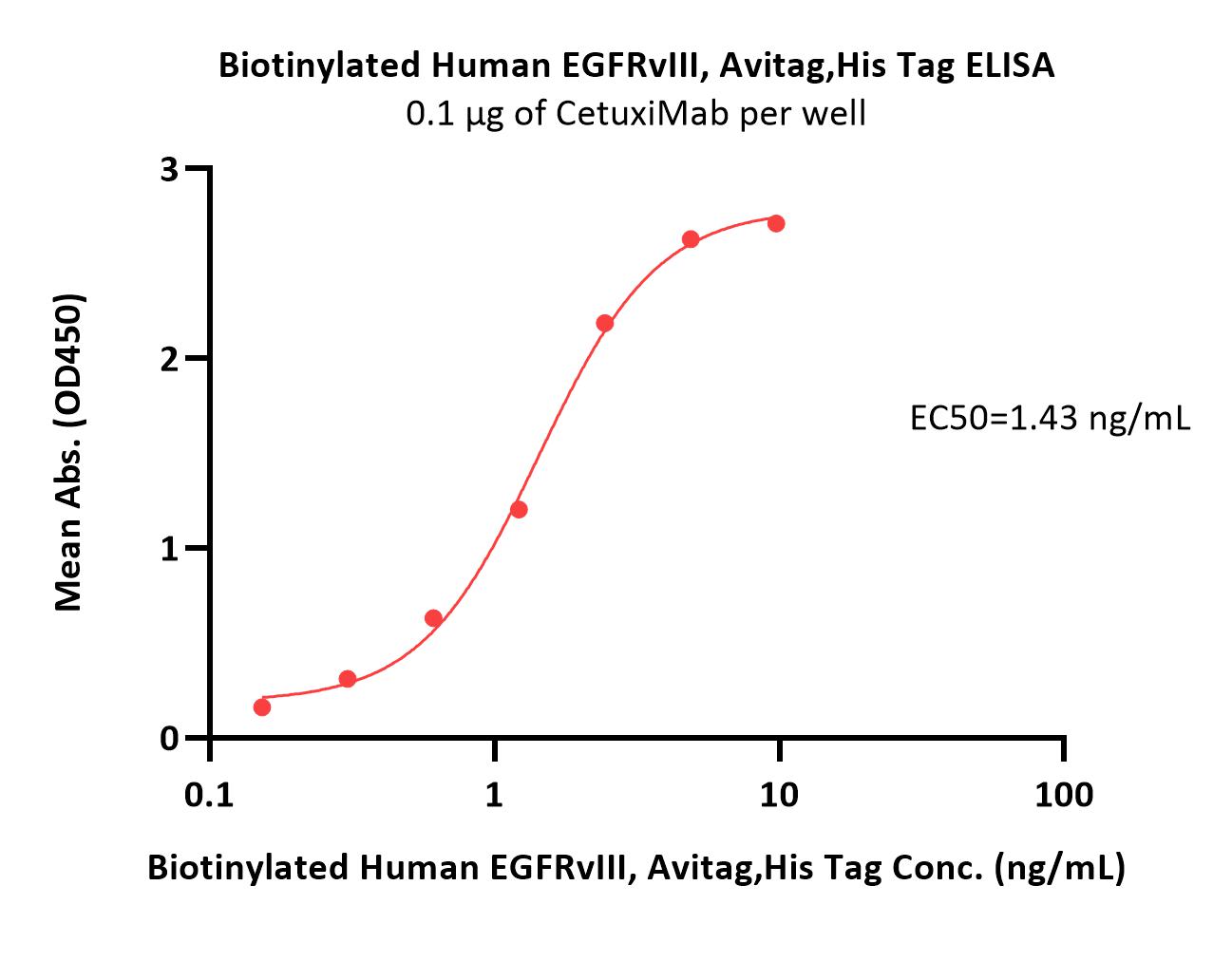
Abstract: A nanoplatform based on self-assembling peptides was developed with the ability to effectively transport and deliver a wide range of moieties across the blood-brain barrier (BBB) for the treatment of glioblastoma. Its surface was functionalized to have a targeted release of TMZ thanks to the targeting peptide that binds to EGFRvIII, which is overexpressed on tumor cells, and gH625, which acts as an enhancer of penetration. Furthermore, the on-demand release of TMZ was achieved through matrix metalloproteinase-9 (MMP-9) cleavage. Nanofibers were characterized for their stability, critical aggregation concentration, and morphology. Next, the effect on both 2D and 3D glioblastoma/astrocytoma (U-87) and glioma (U-118) cell lines was evaluated. The Annexin V/Propidium iodide showed an increase in necrotic and apoptotic cells, and the morphological analysis allowed to discover that both U-118 and U-87 spheroids are smaller in surface, perimeter, and Feret's diameter when treated with NF-TMZ. The developed nanofiber was demonstrated to permeate the BBB in vitro in a 3D spheroidal biodynamic BBB model. Finally, there were no cytotoxic effects of nanofibers without the drug on spheroids, while a significant decrease in viability was observed when NF-TMZ was used. Overall, these results open new opportunities for the evaluation of the efficacy and safety of this nanoplatform in in vivo studies.
Bispecific T-cell engagers for the recruitment of T cells in solid tumors: a literature reviewDewaele, Fernandes
Immunother Adv (2025) 5 (1), ltae005
Abstract: In the past decade, T-cell-based immunotherapies have grown to become some of the most promising treatments for cancer. Following the success of immune checkpoint inhibitors, other T-cell-based therapies emerged including CAR-T cells and bispecific T-cell engagers (BiTEs). BiTEs have the unique ability to crosslink T cells and tumor cells independently of major histocompatibility complex (MHC) restriction. They do not rely on TCR specificity or the CD4+/CD8+ costimulatory molecules, overcoming tumor MHC downregulation and low-affinity TCR binding. However, like many other immunotherapies, BiTEs have shown limited success beyond the treatment of hematological malignancies. BiTEs for the treatment of solid tumors still face challenges. Studies in gastrointestinal tumors have revealed Fc toxicity, short half-lives, and immunotoxicity, leading to Fc-silenced half-life extended BiTEs with humanized single-chain variable fragments. Studies in prostate tumors, lung tumors, and malignant gliomas have identified promising targets in PSMA, DLL3, and EGFRvIII, respectively, but also highlighted the problems of on-target off-tumor and BiTE-specific toxicities and inaccessible or immunosuppressive tumor microenvironments. Ongoing research to overcome these limitations remains an interesting field to follow, as BiTEs have the potential to be a powerful tool, especially when used in combination with other immunotherapies.© The Author(s) 2025. Published by Oxford University Press on behalf of the British Society for Immunology.
A Cross-Sectional Exploratory Study of Rat Sarcoid (Ras) Activation in Women with and Without Polycystic Ovary SyndromeNiinuma, Habib, Takemoto
et alCells (2025) 14 (5)
Abstract: Objective: Rat sarcoma (Ras) proteins, Kirsten, Harvey, and Neuroblastoma rat sarcoma viral oncogene homolog (KRAS, HRAS, and NRAS, respectively), are a family of GTPases, which are key regulators of cellular growth, differentiation, and apoptosis through signal transduction pathways modulated by growth factors that have been recognized to be dysregulated in PCOS. This study explores Ras signaling proteins and growth factor-related proteins in polycystic ovary syndrome (PCOS). Methods: In a well-validated PCOS database of 147 PCOS and 97 control women, plasma was batch analyzed using Somascan proteomic analysis for circulating KRas, Ras GTPase-activating protein-1 (RASA1), and 45 growth factor-related proteins. The cohort was subsequently stratified for BMI (body mass index), testosterone, and insulin resistance (HOMA-IR) for subset analysis. Results: Circulating KRas, and RASA1 did not differ between PCOS and control women (p > 0.05). EGF1, EGFR, and EGFRvIII were decreased in PCOS (p = 0.04, p = 0.04 and p < 0.001, respectively). FGF8, FGF9, and FGF17 were increased in PCOS (p = 0.02, p = 0.03 and p = 0.04, respectively), and FGFR1 was decreased in PCOS (p < 0.001). VEGF-D (p < 0.001), IGF1 (p < 0.001), IGF-1sR (p = 0.02), and PDGFRA (p < 0.001) were decreased in PCOS compared to controls. After stratifying for BMI ≤ 29.9 kg/m2, EGFR FGF8, FGFR1 VEGF-D, IGF1, and IGF-1sR differed (p < 0.05) though EGF1, EGFRvIII, FGF8, FGFR1, and VEGF-D no longer differed; after subsequently stratifying for HOMA-IR, only FGFR1, VEGF-D, IGF1, and IGF-1sR differed between groups (p < 0.05). Conclusions: Several growth factors that activate Ras differ between women with and without PCOS, and when stratified for BMI and HOMA-IR, only FGFR1, VEGF-D, IGF1, and IGF-1sR differed; these appear to be inherent features of the pathophysiology of PCOS.
 +添加评论
+添加评论














































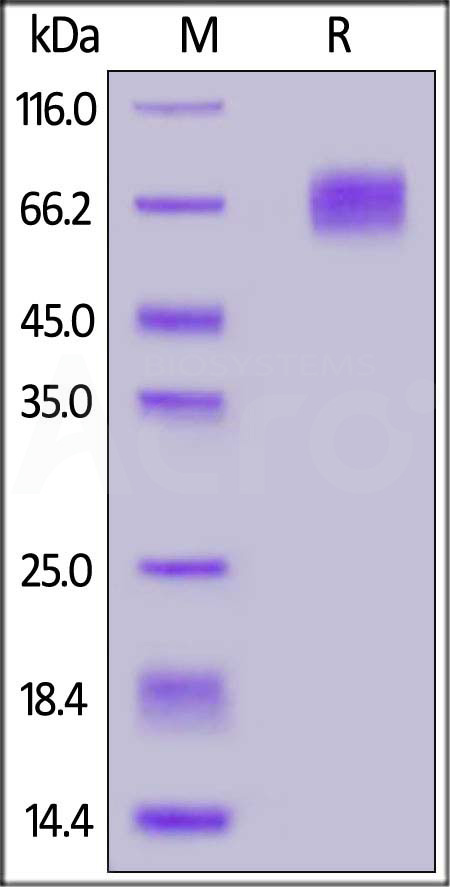
 膜杰作
膜杰作 Star Staining
Star Staining