Optimal injection sites for therapeutic angiogenesis: HGF-mediated regulation of HIF-1α via MAPK/PI3K pathways in hypoxic endothelial cellsWang, Rong, Li
et alTissue Cell (2025) 95, 102871
Abstract: Therapeutic angiogenesis offers a promising strategy for patients with critical limb-threatening ischemia (CLTI) who are unsuitable candidates for revascularization. However, the optimal administration sites for gene therapy agents, such as pCK-HGF-X7, remains undefined. Clinical trials commonly employ multiple intramuscular injections at sites of arterial occlusion; yet the necessity and efficacy of such extensive and repetitive protocols remains unclear. Targeted injections into ischemic tissues or their margins may improve therapeutic outcomes. Moreover, the molecular mechanisms by which hepatocyte growth factor (HGF)/c-Met signaling regulates hypoxia-inducible factor-1α (HIF-1α) expression under hypoxic conditions are not fully understood. This study aims to elucidate these molecular mechanisms in endothelial cells under hypoxic conditions and to identify the most effective injection sites for therapeutic angiogenesis agents. The effects of various HGF isoforms/complexes on human aortic endothelial cells (HAECs) were evaluated under normoxic and hypoxic conditions, focusing on proliferation, migration, and tube formation. Pathway inhibitors were used to explore the underlying mechanisms in hypoxic HAECs, and the findings were validated in a rat hindlimb ischemia model. Results demonstrated that HGF723 and HGF728 activated the mitogen-activated protein kinase (MAPK) and phosphatidylinositol 3-kinase (PI3K) pathways, regulating HIF expression and significantly enhanced endothelial cell proliferation, migration, and tube formation, particularly under hypoxia. Despite these cellular effects, HGF treatment did not significantly improve tissue perfusion or neovascularization in normal rat hindlimbs. However, in ischemic rat hindlimbs, it markedly promoted angiogenesis and improved tissue perfusion in the gastrocnemius muscle. These findings indicate that therapeutic angiogenesis agents should primarily target hypoxic tissues, extending to the interface between normoxic and hypoxic regions, to optimize treatment efficacy.Copyright © 2025 Elsevier Ltd. All rights reserved.
Effects of Chlorella protothecoides-derived polydeoxyribonucleotides on skin regeneration and wound healingPark, Nam, Lee
et alArch Dermatol Res (2025) 317 (1), 483
Abstract: The skin acts as a crucial barrier and, upon injury, initiates complex wound-healing processes involving various cell types. Polydeoxyribonucleotides (PDRNs) are well-known for their efficacy in enhancing skin regeneration and wound healing. This study sought to investigate the effectiveness of PDRNs derived from Chlorella protothecoides, a sustainable and scalable microalgal source, in promoting skin regeneration and wound healing. Keratinocytes and fibroblasts were used for assessing the impact of PDRNs on cell proliferation, migration, collagen synthesis, and angiogenesis. Gene expression and associated signaling pathways were also examined using RT-qPCR and Western blot analyses. Our findings demonstrated that PDRNs significantly enhanced the proliferation and migration of skin cells, upregulated growth arrest specific 6 (GAS6) and hepatocyte growth factor (HGF) expression, and increased collagen synthesis by modulating collagen type I alpha 1 (COLIA1) expression. Additionally, PDRNs enhanced angiogenesis by promoting vascular endothelial growth factor (VEGF) expression and activation of ERK, AKT, β-catenin and STAT3 pathways via an adenosine A2A receptor (A2AR)-dependent mechanism. These findings suggest that microalgal-derived PDRNs have significant potential as sustainable and effective agents for clinical and cosmetic applications aimed at improving skin health and wound healing.© 2025. The Author(s), under exclusive licence to Springer-Verlag GmbH Germany, part of Springer Nature.
Genetic insights into avian influenza resistance in Jeju Island chickens: the roles of Mx1 and oligoadenylate synthetase-like single nucleotide polymorphismsKim, Jeong, Yang
et alJ Anim Sci Technol (2025) 67 (1), 69-85
Abstract: Influenza A virus (FLUAV) causes serious diseases in both poultry and humans. Various host proteins, including Mx1, are considered candidates for avian influenza (AI) resistance. After infecting Jeju Native chicken embryo fibroblasts (CEFs) with three types of AI viruses, we performed gene expression profiling, identified single nucleotide polymorphisms (SNPs) through RNA-sequencing, and confirmed phenotypes showing antiviral activity in vitro. Highly pathogenic AI viruses upregulated FGF2, LYN, and FLT4 and downregulated HGF, ANGPT1, and ROR2, while a low pathogenicity AI upregulated PARK7, RACK1, and DTX3L and downregulated SIRT1, LRRK2, and WAC. However, no virus affected Mx1 expression. Although SNPs in Mx1 could not discriminate antiviral activity alone, the only CEF resistant to H5N6, strain AN4, contained the Mx1 631 R/R genotype and strongly expressed an oligoadenylate synthetase-like (OASL) variant with a unique SNP: c.G880A (p.E294K). Using transfected cell lines, H5N6-infected cells expressing OASL with the c.G880A SNP showed minimal cytopathic effects and the lowest M gene expression. This study confirms that Jeju Native chickens with specific SNP combinations in both Mx1 and OASL showed H5N6 resistance and demonstrates the interplay of genetic factors in host-pathogen dynamics, suggesting a need for integrated analyses of multiple resistance genes to inform AI prevention strategies.© Copyright 2025 Korean Society of Animal Science and Technology.
Super-Resolution Fluorescence Imaging Reveals the Mechanism of NRP1 Clustering on Non-Small-Cell Lung Cancer MembranesLi, Gao, Qi
et alAnal Chem (2025) 97 (4), 2326-2334
Abstract: Neuropilin 1 (NRP1) is upregulated in various types of malignant tumors, especially non-small-cell lung cancer (NSCLC). However, the precise mechanisms for membrane localization and regulation are not fully understood. Observations from super-resolution microscopy have revealed that NRP1 tends to form nanoscale clusters on the cell membrane, with these clusters varying significantly in size and density across different regions. Further research has shown that stimulation by hepatocyte growth factor (HGF) can reorganize the distribution of NRP1, reducing the number of small clusters while promoting the formation of larger ones. This suggests a propensity for internalization after activation. Additionally, dual-color dSTORM imaging has demonstrated a certain degree of colocalization between NRP1 and c-MET, indicating that c-MET plays an important role in stabilizing NRP1 clusters. This study provides new insights into the mechanism behind NRP1's clustered distribution on cell membranes and paves the way for developing more effective therapeutic strategies targeting NRP1 within tumors.

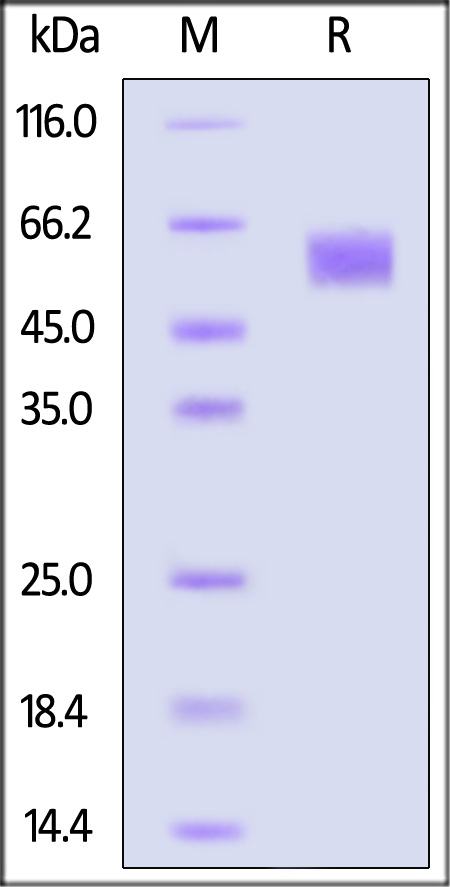


























































 膜杰作
膜杰作 Star Staining
Star Staining