Effects of Space Flight on Inflammasome Activation in the Brain of MiceRoy, Hadad, Rodriguez
et alCells (2025) 14 (6)
Abstract: Space flight exposes astronauts to stressors that alter the immune response, rendering them vulnerable to infections and diseases. In this study, we aimed to determine the levels of inflammasome activation in the brains of mice that were housed in the International Space Station (ISS) for 37 days. C57BL/6 mice were launched to the ISS as part of NASA's Rodent Research 1 Mission on SpaceX-4 CRS-4 Dragon cargo spacecraft from 21 September 2014 to 25 October 2014. Dissected mouse brains from that mission were analyzed by immunoblotting of inflammasome signaling proteins and Electrochemiluminescence Immunoassay (ECLIA) for inflammatory cytokine levels. Our data indicate decreased inflammasome activation in the brains of mice that were housed in the ISS for 37 days when compared to the brains of mice that were maintained on the ground, and in mice corresponding to the baseline group that were sacrificed at the time of launching of SpaceX-4. Moreover, we did not detect any significant changes in the expression levels of the pro-inflammatory cytokines TNF-α, IL-2, IFN-γ, IL-5, IL-6, IL-12p70 and IL-10 between the ground control and the flight groups. Together, these studies suggest that spaceflight results in a decrease in the levels of innate immune signaling molecules that govern inflammasome signaling in the brain of mice.
Immunomodulatory Effect of Rivaroxaban Nanoparticles Alone and in Combination with Sitagliptin on Diabetic Rat ModelElbadr, Galal, Hetta
et alDiseases (2025) 13 (3)
Abstract: Chronic inflammation and immune dysregulation are key drivers of diabetes complications. Rivaroxaban (RX) and sitagliptin (SITA) are established therapies for thromboembolism and glycemic control, respectively. This study evaluated the novel therapeutic potential of nano-rivaroxaban (NRX) alone and in combination with sitagliptin (SITA) in mitigating inflammation and restoring immune balance in streptozotocin (STZ)-induced diabetic rats.Type 2 diabetes was induced in rats using a single injection of STZ (60 mg/kg). Animals were divided into five groups: control, STZ-diabetic, RX-treated (5 mg/kg), NRX-treated (5 mg/kg), and NRX+SITA-treated (5 mg/kg + 10 mg/kg). After 4 weeks of treatment, blood glucose, coagulation markers, pro-inflammatory cytokines (TNF-α, IL-1β, IL-6), and anti-inflammatory cytokines (IL-35, TGF-β1, IL-10) were analyzed. Histopathological examination of the liver, kidney, pancreas, and spleen was conducted. Immunohistochemistry was used to assess hepatic NF-κB expression.STZ significantly elevated pro-inflammatory cytokines (IL-1β, TNF-α, IL-6) and anti-inflammatory cytokines (IL-35, TGF-β1, IL-10), along with increased hepatic NF-κB expression and histopathological abnormalities in immune organs. NRX significantly reduced inflammatory cytokines, improved histopathological changes in organs, and decreased hepatic NF-κB expression. The combination therapy (NRX + SITA) achieved superior immune modulation, with enhanced cytokine profile restoration, reduced hepatic NF-κB expression, and near-complete histopathological normalization.This study underscores the promise of combining nanoparticle-based drug delivery with established therapies like sitagliptin to achieve superior immune modulation and inflammation control, presenting a potential therapeutic strategy for managing diabetes complications.
A Comprehensive Review of Effusive-Constrictive Pericarditis, Diagnosis, and ManagementJamaleddin Ahmad, Ali Abdi, Verma
et alCardiol Rev (2025)
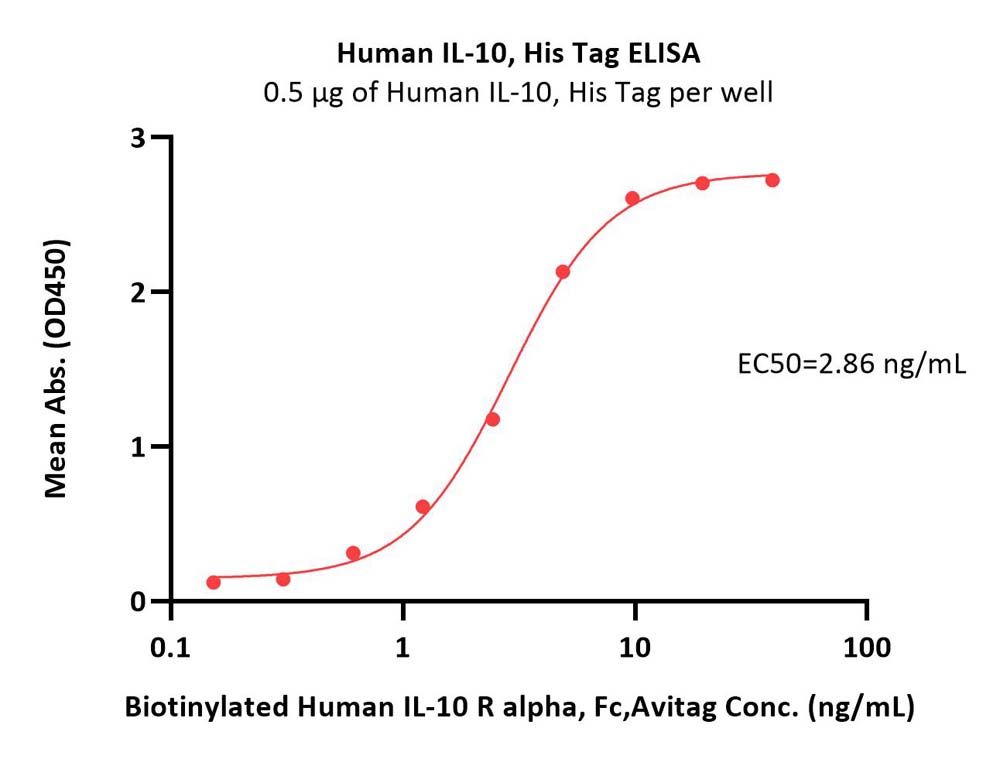
Abstract: Effusive-constrictive pericarditis (ECP) is characterized by fluid accumulation in the pericardial space and a rigid, fibrotic pericardium that restricts heart filling. Its diverse causes include infectious agents, systemic inflammatory conditions, malignancies, and iatrogenic factors. ECP is more prevalent in areas burdened by contagious diseases, such as tuberculous pericardial effusion, and it is found in about 6.7% of patients with tuberculous pericardial effusion. The diagnosis of ECP has improved with advanced imaging techniques, yet challenges persist. Although Doppler echocardiography is sensitive, it lacks specificity, and cardiac catheterization remains the gold standard. Emerging biomarkers such as interleukin-10 may enhance diagnosis, but further validation is needed. Techniques such as cardiac magnetic resonance imaging and computed tomography are used to identify structural abnormalities, but their routine application is still developing. Management of ECP is based on its underlying cause and severity, often starting with pericardiocentesis followed by anti-inflammatory treatments. For severe cases with significant fibrosis, pericardiectomy is the definitive solution. Prognosis varies, with malignancy-related cases typically yielding poorer outcomes than infectious origins. This review explores ECP's pathophysiology, diagnostic challenges, and treatment strategies. It highlights knowledge gaps and suggests future research directions. A multidisciplinary approach is crucial for understanding and improving patient care for this complex condition.Copyright © 2025 Wolters Kluwer Health, Inc. All rights reserved.
Immune Dysregulation in HIV and COVID-19 Co-infection: Therapeutic ImplicationsNejabat, Motamedifar, Fard
et alImmun Inflamm Dis (2025) 13 (3), e70164
Abstract: Co-infection with HIV and SARS-CoV-2 presents a complex clinical picture. Deciphering the immune response in this population, particularly the role of cytokines underlying immunopathogenesis could elucidates the development of targeted therapeutic interventions.This prospective, two-stage study enrolled 75 individuals with HIV diagnosed with COVID-19 (case group) and 25 individuals from the general population infected with SARS-CoV-2 only (control group). COVID-19 diagnosis followed World Health Organization guidelines. Plasma cytokine levels were measured using a cytokine bead array.The case group skewed slightly females (61.2% vs. 42.9% female in the control group) an average age of 3 years older (44.13 years vs. 40.86 years). Importantly, all the case group participants had mild complications, while a significant majority (88.1%) in the control group experienced severe complications. The control group displayed a substantially higher IgM titer 963 IU/mL compared to only 39.3 IU/mL in the case group. The control group had significantly higher levels of IL-6, IL-10, IFN-γ, TNF-α compared to the case group.This study suggests a potentially distinct immune response in HIV-positive patients when infected with SARS-CoV-2. Elucidating these differences could lead to the development of more effective treatment strategies for this vulnerable population.© 2025 The Author(s). Immunity, Inflammation and Disease published by John Wiley & Sons Ltd.

























































 膜杰作
膜杰作 Star Staining
Star Staining















