Protein tyrosine phosphatase delta is a STAT3-phosphatase and suppressor of metabolic liver diseaseRoca Suarez, Jühling, Moehlin
et aleGastroenterology (2025) 3 (1), e100159
Abstract: Impaired hepatic expression of protein tyrosine phosphatase delta (PTPRD) is associated with increased STAT3 transcriptional activity and reduced survival from hepatocellular carcinoma in patients with chronic hepatitis C virus infection. However, the PTPRD-expressing hepatic cell types, signalling pathways responsive to PTPRD and their role in non-viral liver disease are largely unknown.We studied PTPRD expression in single-cell and bulk liver transcriptomic data from mice and humans, and established a Ptprd-deficient mouse model for metabolic dysfunction-associated steatohepatitis (MASH). Identified pathways were validated by perturbation studies in human hepatocytes and PTPRD substrates by pull-down assays. The clinical relevance was further explored in a cohort with metabolic disease by ranking patients according to PTPRD expression and analysing its association with metabolic disease markers.The analysis of individuals ranked according to PTPRD expression and Ptprd-deficient mice, showed that PTPRD levels were associated with hepatic glucose/lipid signalling and peroxisome function. Hepatic PTPRD expression is impaired in aetiologies of chronic liver diseases that are associated with metabolic disease. We further validated PTPRD as a STAT3 phosphatase in the liver, acting as a regulator of peroxisomal fatty acid metabolism. During MASH, low PTPRD led to increased liver steatosis in Ptprd+/- mice and a pronounced unfolded protein response, which impacts insulin signalling. Accordingly, silencing of PTPRD blunted insulin-induced AKT phosphorylation. Patients with obesity and low hepatic PTPRD expression exhibit increased levels of metabolic risk factors.Our data revealed an important regulatory role of the hepatic PTPRD-STAT3 axis in maintaining glucose/lipid homeostasis, which is recapitulated in clinical manifestations of metabolic liver disease.Copyright © Author(s) (or their employer(s)) 2025. Re-use permitted under CC BY-NC. No commercial re-use. See rights and permissions. Published by BMJ Group.
Discovery of mutations predictive of survival benefit from immunotherapy in first-line NSCLC: A retrospective machine learning study of IMpower150 liquid biopsy dataYuan, Feng, Ding
et alComput Biol Med (2025) 189, 109964
Abstract: Predictive biomarker identification in cancer treatment has traditionally relied on pre-defined analyses, limiting discoveries to expected biomarkers and potentially overlooking novel ones predictive of therapy response. In this work, we develop a novel machine-learning approach capable of exploring full landscape of mutations and combinations and identify potentially new predictive biomarkers for chemoimmunotherapy. Utilizing the liquid biopsy dataset from 313 non-small cell lung cancer (NSCLC) patients in the Phase 3 Impower150 trial (NCT02366143), we developed the HRdiffRF algorithm with a novel hazard ratio-splitting criterion. Predictive mutations and combinations were identified for overall survival (OS) improvement with atezolizumab plus bevacizumab plus carboplatin and paclitaxel (ABCP) compared to bevacizumab plus carboplatin and paclitaxel (BCP). Our analysis confirms the predictive role of KRAS mutations and reveals the predictive value of PTPRD and SMARCA4 mutations in chemoimmunotherapy efficacy. Unlike other KRAS wild-type NSCLC patients, NSCLC patients with KRAS wild-type status and mutations in FAT1, ERBB2, or PTPRD may benefit from chemoimmunotherapy, while NTRK3 and GNAS mutations could negatively impact survival. Patients harboring concurrent KRAS and KEAP1 mutations may not benefit from chemoimmunotherapy. These findings highlight the complex genetic factors influencing treatment response for chemoimmunotherapy in NSCLC. In summary, the proposed machine-learning tool identified potential predictive biomarkers for first-line chemoimmunotherapy in NSCLC and can be readily applied to other tumor types and studies. It can also be extended to explore predictive biomarkers beyond mutations.Copyright © 2025. Published by Elsevier Ltd.
p53-regulated SESN1 and SESN2 regulate cell proliferation and cell death through control of STAT3Haidurov, Zheltukhin, Snezhkina
et alCell Commun Signal (2025) 23 (1), 105
Abstract: Sestrin1 and Sestrin2 (SESN1&2) are evolutionarily conserved, stress-responsive proteins that regulate cell growth and viability. The primary target of Sestrins is the mTORC1 protein kinase, an activator of anabolic processes and an autophagy inhibitor. Our previous studies showed that inactivating SESN1&2 in lung adenocarcinoma A549 cells accelerates cell proliferation and confers resistance to cell death without affecting mTORC1 activity, suggesting that SESN1&2 modulate cellular processes via mTORC1-independent mechanisms. This work describes a new mechanism through which SESN1&2 regulate cell proliferation and death by suppressing the STAT3 transcription factor. Normally activated in response to stress and inflammation, STAT3 is frequently overactivated in human cancers. This overactivation promotes the expression of pro-proliferative and anti-apoptotic genes that drive carcinogenesis. We demonstrate that SESN1&2 inactivation stimulates STAT3 by downregulating the PTPRD phosphatase, a protein responsible for STAT3 dephosphorylation. Our study demonstrates that SESN1&2 deficiency may cause STAT3 activation and facilitate carcinogenesis and drug resistance, making SESN1&2 reactivation a potential cancer treatment strategy.© 2025. The Author(s).
Clinicopathologic and Molecular Characterization of Gynecologic Carcinosarcomas With a Mesonephric-Like Carcinomatous ComponentMendoza, Tjota, Choi
et alAm J Surg Pathol (2025)
Abstract: Carcinosarcoma with a mesonephric-like carcinomatous component (MLCS) is a rare subtype of gynecologic malignancy recently described in the literature. This study aims to expand the genomic characterization of MLCS by performing independent molecular analysis of the carcinomatous and sarcomatous components in a series of MLCS. Eight cases of gynecologic MLCS (endometrial, lower uterine segment, and ovarian) were identified and underwent clinicopathologic evaluation. Genomic DNA extraction and next-generation sequencing (NGS) were performed separately from the carcinomatous and sarcomatous components of 4 tumors, while 2 tumors underwent NGS of combined carcinomatous and sarcomatous components. The average age at diagnosis was 65.6 years (range 50 to 83 years). MLCS patients were diagnosed at FIGO stage I (n=3), stage II (n=2), stage III (n=2), and stage IV (n=1). The carcinomatous and sarcomatous components were observed to harbor the same single nucleotide variations. All cases had less than 10 mutations/Mb and were microsatellites stable. All cases (6/6, 100%) harbored KRAS point mutations in codon 12, including the following variants: p.G12D (n=2), p.G12A (n=2), and p.G12V (n=2). Five cases showed additional alterations in ARID1A (case 1), PTEN (case 2), PIK3CA (case 4), SPOP (case 6), TET1 (case 6), BUB1 (case 7), LYN (case 7) and PTPRD (case 7). The presence of both KRAS and PTEN/PIK3CA alterations suggests a combined endometrioid and mesonephric differentiation in MLCS.Copyright © 2025 Wolters Kluwer Health, Inc. All rights reserved.

 +添加评论
+添加评论















































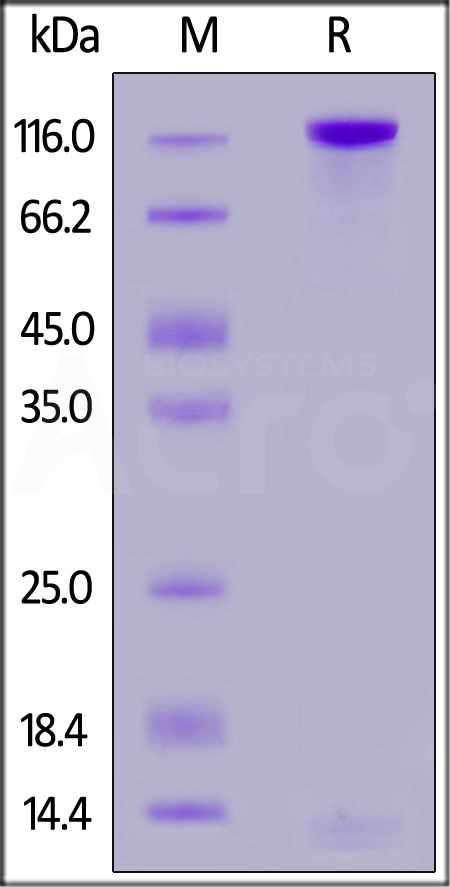
 膜杰作
膜杰作 Star Staining
Star Staining