Colorectal Cancer: Risk Factors, Novel Approaches in Molecular Screening and TreatmentAnbari, Ghanadi
Int J Mol Cell Med (2025) 14 (1), 576-605
Abstract: By 2040 the burden of colorectal cancer will increase to 3.2 million new cases per year and 1.6 million deaths per year. This highlights the importance of improving preventive measures and treatment strategies. This piece concisely overviews the latest therapeutic and diagnostic approaches for colorectal cancer. In 2019, factors such as low milk intake, smoking, insufficient calcium consumption, and alcohol use had a significant impact on colorectal cancer DALYs worldwide. A comprehensive search was conducted in December 2023 using keywords related to drugs, therapeutic agents, colorectal cancer, diagnostic methods, epidemiology, and novel therapeutic approaches in the PubMed and Scopus databases. Initially, 325 articles were identified based on titles, abstracts, and publication dates. After removing duplicates, 170 unique articles were included. Medications like Nimotuzumab, Cetuximab, and Panitumumab target the Epidermal Growth Factor Receptor (EGFR), which EGF activates. HER2, activated by ligands, is the focus of drugs like Trastuzumab and Pertuzumab. The PD-1/PD-L1 and CTLA-4 pathways, as the immune checkpoints, which involve T cells, are targeted by medications like Ipilimumab. Adoptive cell therapy, including CAR-T cell therapy, TCR modification, and enhancing T cell activity through tumor-infiltrating lymphocytes, is used to combat cancer cell growth. In medical advancements, adoptive cell transfer therapy (ACT) and exosomes in the tumor immune microenvironment (TME) are notable treatment methods that boost the immune system. HIF1A-AS1, CRNDE-h, NEAT1, ZFAS1, and GAS5, along with IGFBP-2, have demonstrated significant CRC diagnostic capacity. Compared to CRC patients with low HIF1A-AS1 expression, individuals with high expression levels were linked to a worse 5-year survival rate.© The Author(s).
Determination of both the expression and serum levels of epidermal growth factor and transforming growth factor β1 genes in COVID-19Yildiz Gulhan, Eroz, Ozturk
et alSci Rep (2025) 15 (1), 9771
Abstract: We aimed to evaluate the effects of both the expression and serum levels of Epidermal growth factor (EGF) and Transforming growth factor-β1 (TGF-β1) genes in patients with different degrees of cellular damage as mild, moderate, severe, and critical illness that can lead to fibrosis caused by SARS-CoV-2. Totally 45 individuals (male: 21(46.67%); female: 24(53.33%)) with COVID-19 infection were included in this study. Four groups were constituted as mild (n = 16)], moderate (n = 10), severe (n = 10), and critical (n = 9) according to the severity of the disease. Blood samples were drawn from the patients, and all of the hemograms, EGF and TGFβ1 gene expression, and serum levels were evaluated. The mean age of individuals was 57.311 ± 18.383 (min: 28, max: 94). Significant differences were found among the groups for PLT (χ2 = 9.955; p = 0.019), CRP (χ2 = 7.693; p = 0.053), Ferritin (χ2 = 22.196; p < 0.001), D-dimer (χ2 = 21.982; p = 0.000), LDH (χ2 = 21.807; p < 0.001) and all these parameters (exclude PLT in severe groups) was increased depending on the severity of the disease. Additionally, significant differences were detected for EGF (χ2 = 29.528; p < 0.001), TGFB1 (χ2 = 28.981; p < 0.001) expression (that increased depending on the disease severity), and EGF (χ2 = 7.84; p = 0.049), TGFB1 (χ2 = 17.451; p = 0.001) serum concentration levels (that decreased depending on the disease severity). This study found statistically significant differences for both EGF 2-ΔΔCt. TGFβ1 2-ΔΔCt and EGF, TGFβ1 serum concentration values among all patient groups. As disease severity increased, EGF 2-ΔΔCt. TGFβ1 2-ΔΔCt levels increased, while EGF and TGFβ1 serum concentration levels decreased. Perhaps this study will be useful in managing COVID-19 infection severity and pulmonary fibrosis cases secondary to COVID-19.© 2025. The Author(s).
Modulation of Intestinal Signal Transduction Pathways: Implications on Gut Health and DiseaseVerma, Garg, Yadav
et alEur J Pharmacol (2025)
Abstract: The gastrointestinal (GI) tract is essential for nutrient absorption and protection against pathogens and toxins. Its epithelial lining undergoes continuous renewal every 3-5 days, driven by intestinal stem cells (ISCs). ISCs are primarily of two types: actively proliferating crypt base columnar cells (CBCs), marked by Lgr5 expression, and quiescent label-retaining cells (+4 LRCs), which act as reserves during stress or injury. Key signaling pathways, such as Wnt/β-catenin, Notch, bone morphogenetic proteins (BMPs), and epidermal growth factor (EGF), are crucial in maintaining epithelial homeostasis. These pathways regulate ISCs proliferation and their differentiation into specialized epithelial cells, including goblet cells, paneth cells, enteroendocrine cells, and enterocytes. Disruptions in ISCs signaling can arise from extrinsic factors (e.g., dietary additives, heavy metals, pathogens) or intrinsic factors (e.g., genetic mutations, metabolic changes). Such disruptions impair tight junction integrity, induce inflammation, and promote gut dysbiosis, often perpetuating a cycle of intestinal dysfunction. Chronic ISCs dysregulation is linked to severe intestinal disorders, including colorectal cancer (CRC) and inflammatory bowel disease (IBD). This review emphasizes the critical role of ISCs in maintaining epithelial renewal and how various factors disrupt their signaling pathways, jeopardizing intestinal health and contributing to diseases. It also underscores the importance of protecting ISCs function to mitigate the risk of inflammation-related disorders. It highlights how understanding these regulatory mechanisms could guide therapeutic strategies for preserving GI tract integrity and treating related conditions.Copyright © 2025. Published by Elsevier B.V.
KBU2046 exerts inhibition on chemokine gradient-mediated motility of esophageal squamous cell carcinoma through reducing integrin expressionLi, Chen, Li
et alBiochim Biophys Acta Mol Basis Dis (2025)
Abstract: Esophageal squamous cell carcinoma (ESCC) cells migrate from their initial site of origin, ultimately forming metastasis and causing death. The selective inhibition of ESCC cell movement has not been possible to date. Here we demonstrate that the small molecule therapeutic agent KBU2046 inhibits the characteristic migration and invasion of ESCC cells induced by chemokine gradients, having no effect on cell proliferation. After demonstrating that KBU2046 inhibits human ESCC metastasis in a murine model, we showed that it doesn't inhibit the in vitro efficacy of chemotherapeutic agents used clinically, going on to demonstrate maintenance of cisplatin efficacy when combined with KBU2046 in a murine model. Mechanistic studies demonstrated that KBU2046 inhibited epidermal growth factor (EGF)-mediated phosphorylation of receptor-interacting serine/threonine protein kinase 1 (RIPK1) on its Ser166 activation motif. RIPK1 was shown to be necessary for KBU2046 efficacy. However, this was shown to be dependent upon cell context, and was also shown to be dependent upon level of RIPK1 expression, both supporting the presence of additional therapeutically sensitive regulatory pathways. Mass spectrometry analysis of ESCC cells demonstrated that KBU2046 selectively altered the expression of proteins involved in cell motility. Integrin αV (ITGAV) is overexpressed in ESCC, was decreased by KBU2046, and its knockdown inhibited ESCC cell migration and invasion, which was necessary for KBU2046 efficacy. We demonstrate that ESCC's motility can be inhibited, and KBU2046 inhibits motility in an Integrin αV-dependent manner, and that combining anti-motility and cytotoxic agents is a high value therapeutic strategy for ESCC that should be further developed.Copyright © 2025. Published by Elsevier B.V.



 +添加评论
+添加评论






















































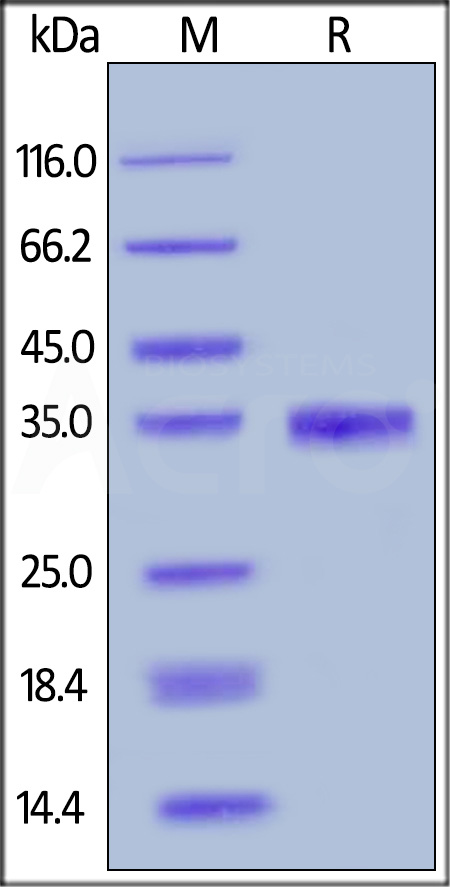
 膜杰作
膜杰作 Star Staining
Star Staining