HLA-Region Genetic Association Analysis of Breast Cancer Patients With and Without Persistent Postsurgical Neuropathic PainMustonen, Nieminen, Koskela
et alEur J Pain (2025) 29 (4), e70009
Abstract: Surgical nerve injuries lead to persistent neuropathic pain (NP) in up to 30% of patients. Among many other factors, polymorphisms in the human leukocyte antigen (HLA) genes have been suggested to contribute to the development of neuropathic pain.We performed a genetic association analysis of HLA class I and class II alleles in women who had been operated on for breast cancer. Patients had a surgeon-confirmed perioperative nerve injury and were examined 4-9 years after their surgery. Patients with painful (cases, n = 27) and painless (controls, n = 30) intercostobrachial nerve resection were studied. Cases included patients with definite NP with worst pain intensity in the past week ≥ 4/10 on a numerical rating scale (NRS) and controls had the same nerve injury with no NP or other pains. Whole-genome single nucleotide polymorphism data were produced, and HLA class I (HLA-A, -B, -C) and class II (HLA-DRB1, -DQA1, -DQB1 and -DPB1) alleles were determined by imputation.HLA-DRB1*03:01, DQA1*05:01 and DQB1*02:01 alleles appeared to be associated with painful nerve injury after breast cancer surgery (nominal p = 0.007 for all, carriership OR = 12.0, 95% CI 1.38-104; FDR corrected p > 0.07). These alleles comprise the DR3-DQ2 haplotype, which is part of the ancestral haplotype AH8.1.Our results provide further support for the role of HLA genetic variation in the development of persistent post-surgical neuropathic pain, which indirectly implies a mechanism involving immunological memory in this process.We report a novel association between the HLA-DR3-DQ2 haplotype and the development of persistent neuropathic pain after breast cancer surgery. Our results provide further evidence for the role of HLA polymorphism in persistent neuropathic pain.© 2025 European Pain Federation ‐ EFIC ®.
Pharmacological manipulation of liver fibrosis progression using novel HDAC6 inhibitorsBorrello, Ruzic, Paish
et alFEBS J (2025)
Abstract: Chronic liver injury characterized by unresolved hepatitis leads to fibrosis, potentially progressing to cirrhosis and hepatocellular carcinoma. Effective treatments for halting or reversing liver fibrosis are currently lacking. This study investigates the potential of HDAC6 as a therapeutic target in liver fibrosis. We synthesized two selective HDAC6 inhibitors, DR-3 and FDR2, and assessed their effects on hepatic stellate cell (HSC) activation and liver fibrosis using human precision cut liver slices (hPCLS). Molecular docking, deacetylation inhibition assays, and various cellular assays were employed to evaluate the specificity and anti-fibrotic efficacy of these inhibitors. DR-3 and FDR2 demonstrated high selectivity for HDAC6 over HDAC1, significantly inhibiting HSC activation markers and fibrogenic gene expression. Both inhibitors increased acetylation of α-tubulin and suppressed TGF-β1-induced SMAD signaling in HSCs. In human precision cut liver slices (hPCLS), DR-3 and FDR2 reduced fibrogenic protein levels and collagen deposition. The selective inhibition of HDAC6 by DR-3 and FDR2 effectively reduces HSC activation and fibrogenesis in liver models, supporting further investigation of HDAC6 inhibitors as potential anti-fibrotic therapies.© 2025 The Author(s). The FEBS Journal published by John Wiley & Sons Ltd on behalf of Federation of European Biochemical Societies.
Two DRB3 residues predictively associate with the progression to type 1 diabetes among DR3 carriersZhao, Papadopoulos, Skyler
et alJCI Insight (2025)
Abstract: HLA-DR genes are associated with the progression from stage 1 and stage 2 to onset of stage 3 type 1 diabetes (T1D), after accounting HLA-DQ genes with which they are in high linkage-disequilibrium. Based on an integrated cohort of participants from two completed clinical trials, this investigation finds that sharing a haplotype with the DRB1*03:01 (DR3) allele, DRB3*01:01:02 and *02:02:01 have respectively negative and positive associations with the progression. Further, we uncovered two residues (β11, β26, participating in pockets 6 and 4, respectively) on the DRB3 molecule responsible for the progression among DR3 carriers, i.e. motif RY and LF respectively delay and promote the progression (Hazard Ratio = 0.73 and 2.38, p-value = 0.039 and 0.017, respectively). Two anchoring pockets 6 and 4 probably bind differential autoantigenic epitopes. We further investigated the progression association with the motifs RY and LF among carriers of DR3 and found that carriers of the motif LF have significantly faster progression than carriers of RY (HR = 1.48 and p = 0.019 in unadjusted analysis; HR = 1.39, p = 0.047 in adjusted analysis). New insights provide an impetus to examine the possible role of specific DRB3-binding peptides in the progression to T1D.
TL1A, a novel alarmin in airway, intestinal, and autoimmune disordersVarricchi, Poto, Criscuolo
et alJ Allergy Clin Immunol (2025)
Abstract: The term alarmin denotes a broad class of molecules rapidly released to alert the immune system through the engagement of specific receptors on immune cells. Three alarmin cytokines-thymic stromal lymphopoietin, IL-33, and IL-25-are released from epithelial and certain stromal cells. TNF-like cytokine 1A (TL1A) is a member of the TNF cytokine superfamily, first identified in human endothelial cells. TL1A is now considered a novel alarmin expressed by human and mouse bronchial and intestinal epithelial cells. TL1A exerts its biological activities by binding to a trimeric receptor DR3 (death receptor 3), expressed on a wide spectrum of immune and structural cells, including lung fibroblasts, endothelial cells, and bronchial epithelial cells. TL1A has been implicated in experimental and human inflammatory bowel diseases as well as in airway inflammation and remodeling in severe asthma. A monoclonal antibody anti-TL1A (tulisokibart) is effective in inducing clinical remission in ulcerative colitis patients. Increasing evidence suggests that TL1A is also involved in certain autoimmune disorders, such as rheumatoid arthritis and psoriasis. These emerging findings broaden the role of TL1A in various human inflammatory conditions. Several clinical trials are currently evaluating the safety and efficacy of monoclonal antibodies targeting TL1A in asthma or inflammatory bowel disease patients.Copyright © 2025 The Authors. Published by Elsevier Inc. All rights reserved.

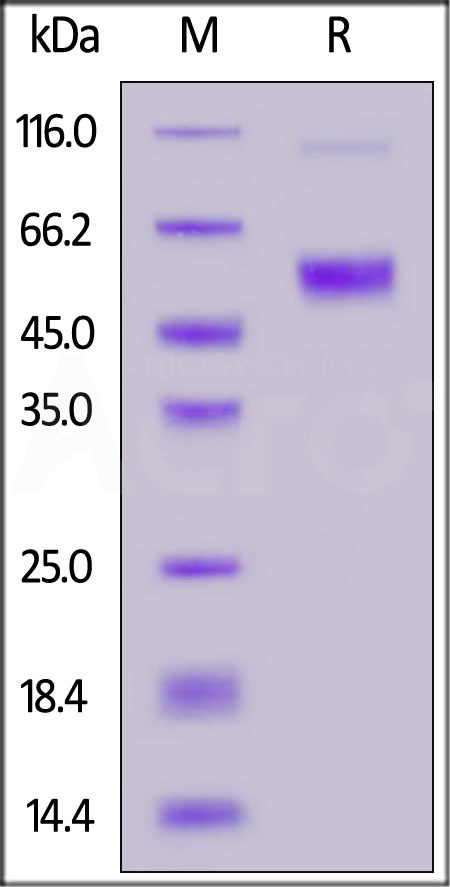























































 膜杰作
膜杰作 Star Staining
Star Staining
















