[Update on cardiovascular prevention 2025]Wienbergen, Hanses, Kerniss
et alHerz (2025)
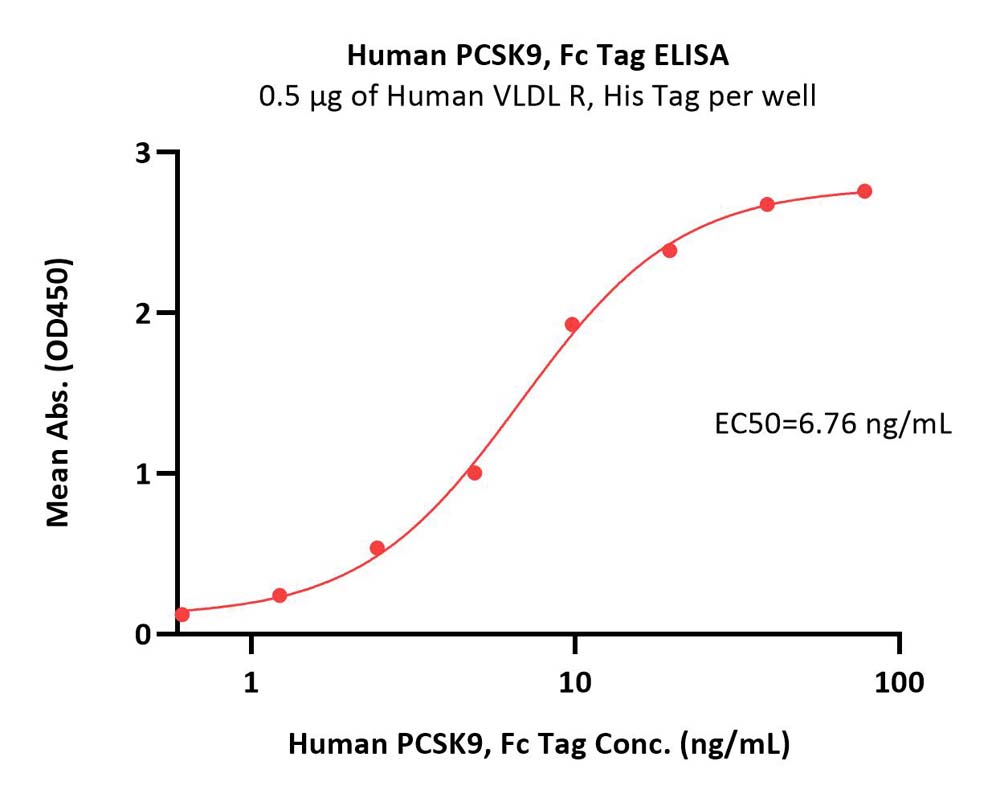
Abstract: Despite an expensive healthcare system Germany performs poorly with respect to life-expectancy compared to other countries, for which cardiovascular diseases and deficits in cardiovascular prevention in particular are responsible. The basis of cardiovascular prevention is a healthy lifestyle with regular physical exercise, a predominantly plant-based diet, nonsmoking, good sleep and mental health. In many cases additional lipid-lowering, antidiabetic and antihypertensive medications are necessary. Recent studies have proven the prognostic effects of different groups of medications, such as proprotein convertase subtilisin/kexin type 9 (PCSK9) inhibitors, sodium-glucose transporter 2 (SGLT2) inhibitors and glucagon-like peptide 1 (GLP-1) receptor agonists, in the appropriate indication areas. To improve the cardiovascular prevention in Germany, intensified public efforts are crucial. In addition, individual support of patients is effective for long-term preventive measures. To achieve this healthcare professionals must be trained (physicians, cardiovascular prevention assistants), who can sustainably support patients in lifestyle modifications and medicinal prevention.© 2025. The Author(s), under exclusive licence to Springer Medizin Verlag GmbH, ein Teil von Springer Nature.
Association between statin discontinuation after proprotein convertase subtilisin/kexin type 9 inhibitor initiation and subsequent atherosclerotic cardiovascular disease eventsPeasah, Lee, Do
et alJ Manag Care Spec Pharm (2025) 31 (4), 377-385
Abstract: Clinical guidelines recommend the use of proprotein convertase subtilisin/kexin type 9 inhibitors (PCSK9is) in patients with atherosclerotic cardiovascular disease (ASCVD) and nonoptimal low-density lipoprotein.To evaluate the association between discontinuation of statin use after PCSK9i initiation and subsequent ASCVD events.This pre-post retrospective comparative study used national administrative data of adult statin medication users (age ≥18 years) with an index PCSK9i claim (January 1, 2019, to April 30, 2021), prior ASCVD diagnosis, and a 2-year follow-up period. Proportions and probability of ASCVD events post-index (PCSK9i) vs pre-index (PCSK9i) for patients who discontinued statins (discontinued cohort) and those who continued statins (continued cohort) were compared. Propensity score weighting was used to balance patient baseline characteristics. Multivariate Poisson regression and time-to-event Cox regression models were used to assess the association between statin discontinuation and ASCVD events.There were 294 and 46 patients in the continued and discontinued cohorts, respectively. Unweighted results showed that patients in the continued cohort were more likely to receive high-intensity statins (32% vs 22%; P = 0.4) and have a Charlson Comorbidity Index score of 3 or more (62% vs 54%; P = 0.5) at baseline. Baseline statin adherence was lower in the discontinued cohort (6.7% vs 59%; P < 0.001) but 30% each in the propensity 1:1 matched cohort. The 2 cohorts (after matching) had similar ASCVD event prevalence (discontinued cohort: 24% vs continued cohort: 26%) in the baseline and the same lower prevalence (6.5% each; P > 0.9) in the 24-month follow-up period. The odds of any ASCVD event post-index was comparable between the 2 cohorts (reference: continued cohort; odds ratio = 1.88; 95% CI = 0.28-14.6; P = 0.51). There were no statistically significant differences between the 2 groups in the Cox regression (P = 0.47).Post-ASCVD event rates were significantly lower in both cohorts, but discontinuation of statins was not associated with unfavorable ASCVD outcomes.
Early Changes in the Plasma Lipidome of People at Very High Cardiovascular Risk: A New Approach to Assessing the Risk of Cardiovascular ChangesWaś, Dobrowolski, Prejbisz
et alBiomedicines (2025) 13 (3)
Abstract: Background/Objectives: Cardiovascular disease (CVD) remains the leading cause of death worldwide and requires a deeper understanding of its pathogenesis for effective prevention and treatment. Familial hypercholesterolemia (FH), characterized by high levels of LDL cholesterol, is a significant risk factor for CVD. FH background remains unexplained despite advances in genetic testing. The aim was identification early changes in the plasma lipidome of individuals at high cardiovascular risk (HCVR) using liquid chromatography coupled with mass spectrometry. Methods: The lipidomic analysis examined over 400 compounds. Twenty individuals with suspected FH, very high cardiovascular risk (VHCVR), and undetectable mutations in the LDLR, APOB, or PCSK9 genes were compared to control group in a qualitative-quantitative analysis. Results: Multivariate analyses revealed statistically significant alterations in glycerophospholipids (GC), with a notable increase in phosphatidylcholines ((O-36:0/16:0), OR (95% CI): 1.246 (1.042-1.490), p = 0.0157), phosphatidylethanolamines ((O-40:7/22:6), OR (95% CI): 1.119 (1.039-1.205), p = 0.0028), and phosphatidylglycerol ((40:8/20:4), OR (95% CI): 1.053 (1.008-1.101), p = 0.0219) only in patients with HCVR. These changes, particularly in major classes of GC, underscored their potential as biomarkers for early assessment of cardiovascular risk. Lipidomic profiling revealed associations between specific lipid species and the comorbidities of arterial hypertension, atherosclerosis, and insulin resistance, implicating their role in atherosclerotic cardiovascular disease (ASCVD). Conclusions: This study points early changes in the plasma lipidome in individuals at HCVR, underline potential biomarkers, therapeutic targets for ASCVD, and offer opportunities to improve ASCVD diagnosis, therapy, and risk management strategies through detailed personalized medical approach.
The Role of Cholesterol Metabolism and Its Regulation in Tumor DevelopmentWu, Song, Su
et alCancer Med (2025) 14 (7), e70783
Abstract: Within the tumor microenvironment, tumor cells undergo metabolic reprogramming of cholesterol due to intrinsic cellular alterations and changes in the extracellular milieu. Furthermore, cholesterol reprogramming within this microenvironment influences the immune landscape of tumors, facilitating immune evasion and consequently promoting tumorigenesis. These biological changes involve modifications in numerous enzymes associated with cholesterol uptake and synthesis, including NPC1L1, SREBP, HMGCR, SQLE, and PCSK9.This review systematically summarizes the role of cholesterol metabolism and its associated enzymes in cancer progression, examines the mechanisms through which dysregulation of cholesterol metabolism affects immune cells within the tumor microenvironment, and discusses recent advancements in cancer therapies that target cholesterol metabolism.Targeting cholesterol metabolism-related enzymes can inhibit tumor growth, reshape immune landscapes, and rejuvenate antitumor immunity, offering potential therapeutic avenues in cancer treatment.© 2025 The Author(s). Cancer Medicine published by John Wiley & Sons Ltd.


























































 膜杰作
膜杰作 Star Staining
Star Staining