Engineered Hollow Nanocomplex Combining Photothermal and Antioxidant Strategies for Targeted Tregs Depletion and Potent Immune Activation in Tumor ImmunotherapySun, Wang, Ren
et alAdv Healthc Mater (2025)
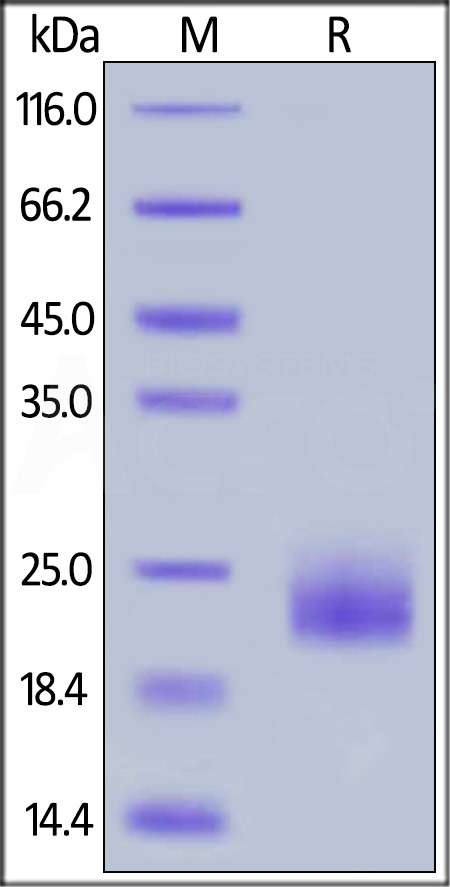
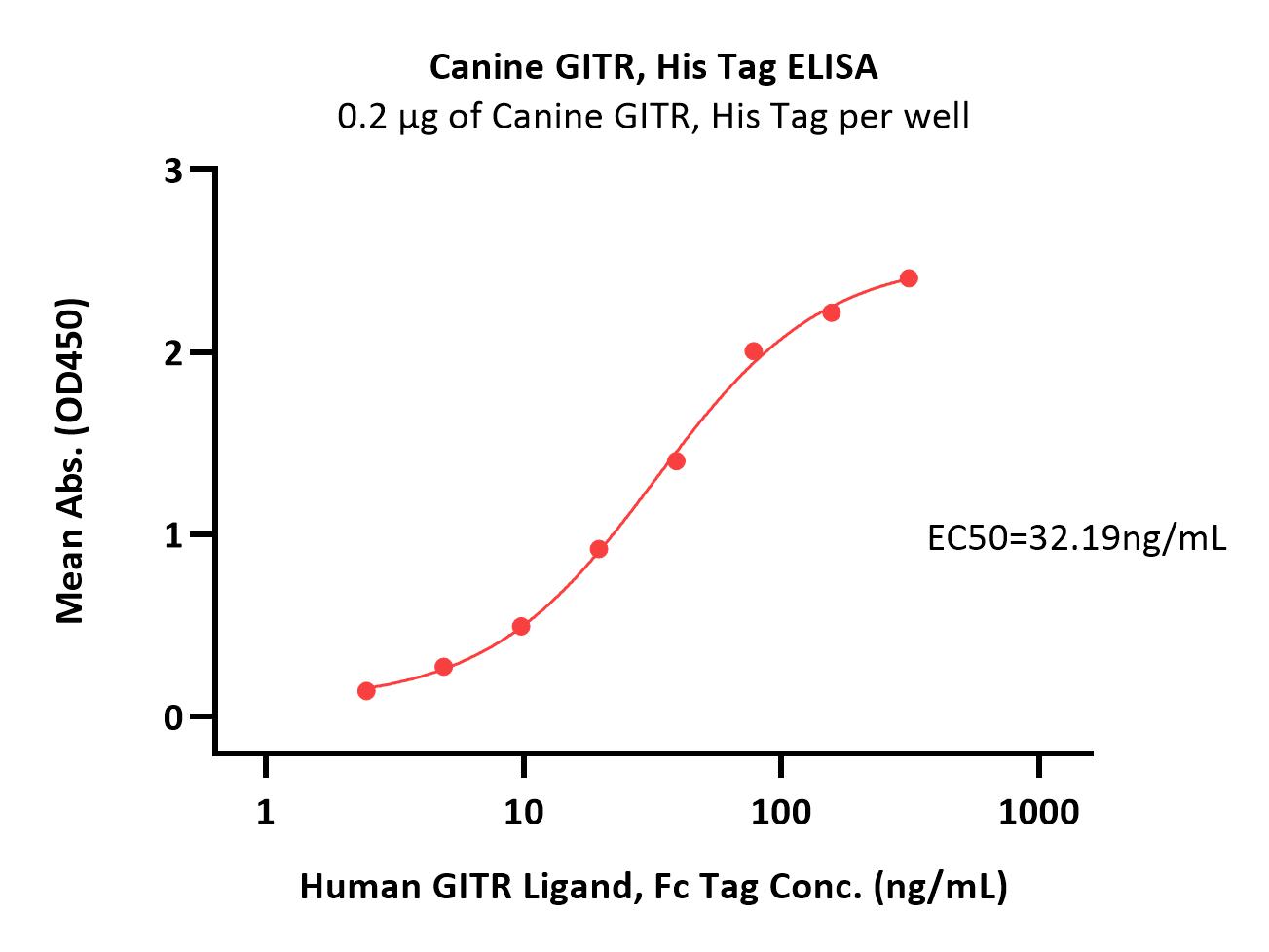
Abstract: In the tumor immunosuppressive microenvironment (TIME), regulatory T cells (Tregs) critically suppress anticancer immunity, characterized by high expression of glucocorticoid-induced TNF receptor (GITR) expression and sensitivity to reactive oxygen species (ROS). This study develops a near-infrared (NIR)-responsive hollow nanocomplex (HPDA-OPC/DTA-1) using hollow polydopamine nanoparticles (HPDA), endowed with thermogenic and antioxidative properties, specifically targeting Tregs to activate antitumor immunity. The GITR agonist DTA-1, combined with the antioxidant oligomeric proanthocyanidins (OPC) to deplete Tregs. However, Tregs depletion alone may not sufficiently trigger robust immune responses. The HPDA nanocarrier enhances thermogenic and antioxidative capacities, supporting photothermal immunotherapy. The HPDA-OPC/DTA-1 demonstrates NIR responsiveness for both photothermal therapy (PTT) and OPC release, while facilitating Tregs depletion via DTA-1 and reducing ROS levels, thereby reviving antitumor immunity. Notably, intratumoral CD4+CD25+FOXP3+ Tregs exhibited a 4.08-fold reduction alongside a 49.11-fold increase in CD8+ T cells/Tregs relative to controls. Enhanced dendritic cells (DCs) maturation and immunogenic cell death (ICD) induction further demonstrate that HPDA-OPC/DTA-1 alleviates immunosuppression and activates antitumor immunity. Ultimately, the observed tumor inhibitory effect (tumor volume: 6.75-fold versus the control) and an over 80% survival rate highlight the therapeutic potential of combining Tregs targeting, antioxidant strategy, and photothermal immunotherapy for effective cancer treatment.© 2025 Wiley‐VCH GmbH.
Policymaker and stakeholder perspectives on determinants of fertility decisions through changing environmental and economic conditions in GreenlandPeterson, Rosing, Reimer
et alHealth Place (2025) 92, 103443
Abstract: This study explored linkages between natural resources and determinants of fertility decisions in Greenland. Interviews were conducted with 26 policymakers and key stakeholders in two communities about climate adaptation, hunting and fishing, economic development, and fertility and reproductive health. Participants link fertility outcomes to disparate community socioeconomic circumstances that affect individual access to education and financial mobility. Workforce and education challenges in Greenland limit ability to expand culturally grounded reproductive healthcare. Coordinating healthcare, education, and housing policy may improve material resources to support fertility decisions in Greenland. We contextualize drivers of fertility decisions within Greenland's climate adaptation policy options.Copyright © 2025 The Authors. Published by Elsevier Ltd.. All rights reserved.
Soluble immune checkpoints are dysregulated in patients with sickle cell disease and correlate with inflammatory mediators, autoantibodies, immune cell profiles, and clinical outcomesLi, Pucka, Houran
et almedRxiv (2025)
Abstract: Sickle cell disease (SCD) is a chronic condition characterized by inflammation, immune dysregulation, and debilitating pain.This study investigates soluble immune checkpoints (sICPs) and their associations with inflammatory mediators, immune cell profiles, autoantibodies, and clinical outcomes in SCD.Peripheral blood samples from 50 SCD patients and 40 demographic-matched healthy controls (HCs) were analyzed for 37 sICPs, 80 inflammatory mediators, and 18 autoantibodies using multiplex assays, alongside immune cell profiles via flow cytometry. Pain and quality of life (QoL) were assessed through patient-reported outcome measures (PROMs).Twenty-three sICPs, including arginase-1, BTLA, CD27, CD28, CD47, CD80, CD96, CD134, CD137, CD152, GITR, HVEM, IDO, LAG-3, MICA, MICB, Nectin-2, PD-1, Siglec-7, Siglec-9, TIM-3, TIMD-4, and VISTA, were significantly elevated in SCD patients compared to HCs. These sICPs correlated with multiple proinflammatory mediators (e.g., IL-18), autoantibodies (e.g., MPO), and immune cell activation markers (e.g., CD38/HLA-DR on CD8 T cells). Notably, CD28, CD152, HVEM, and VISTA were strongly associated with systemic inflammation and immune cell activation, while BTLA, LAG-3, PD-1, and CD80 correlated with pain and anxiety scores and QoL.This study highlights complex interactions between sICPs, immune activation, inflammation, and clinical outcomes in SCD, underscoring their potential as biomarkers or therapeutic targets to alleviate inflammation and improve QoL in this challenging clinical population.
RNA neoantigen vaccines prime long-lived CD8+ T cells in pancreatic cancerSethna, Guasp, Reiche
et alNature (2025)
Abstract: A fundamental challenge for cancer vaccines is to generate long-lived functional T cells that are specific for tumour antigens. Here we find that mRNA-lipoplex vaccines against somatic mutation-derived neoantigens may solve this challenge in pancreatic ductal adenocarcinoma (PDAC), a lethal cancer with few mutations. At an extended 3.2-year median follow-up from a phase 1 trial of surgery, atezolizumab (PD-L1 inhibitory antibody), autogene cevumeran1 (individualized neoantigen vaccine with backbone-optimized uridine mRNA-lipoplex nanoparticles) and modified (m) FOLFIRINOX (chemotherapy) in patients with PDAC, we find that responders with vaccine-induced T cells (n = 8) have prolonged recurrence-free survival (RFS; median not reached) compared with non-responders without vaccine-induced T cells (n = 8; median RFS 13.4 months; P = 0.007). In responders, autogene cevumeran induces CD8+ T cell clones with an average estimated lifespan of 7.7 years (range 1.5 to roughly 100 years), with approximately 20% of clones having latent multi-decade lifespans that may outlive hosts. Eighty-six percent of clones per patient persist at substantial frequencies approximately 3 years post-vaccination, including clones with high avidity to PDAC neoepitopes. Using PhenoTrack, a novel computational strategy to trace single T cell phenotypes, we uncover that vaccine-induced clones are undetectable in pre-vaccination tissues, and assume a cytotoxic, tissue-resident memory-like T cell state up to three years post-vaccination with preserved neoantigen-specific effector function. Two responders recurred and evidenced fewer vaccine-induced T cells. Furthermore, recurrent PDACs were pruned of vaccine-targeted cancer clones. Thus, in PDAC, autogene cevumeran induces de novo CD8+ T cells with multiyear longevity, substantial magnitude and durable effector functions that may delay PDAC recurrence. Adjuvant mRNA-lipoplex neoantigen vaccines may thus solve a pivotal obstacle for cancer vaccination.© 2025. The Author(s).
























































 膜杰作
膜杰作 Star Staining
Star Staining
















