Angiogenesis in Glioblastoma-Treatment ApproachesNowacka, Śniegocki, Smuczyński
et alCells (2025) 14 (6)
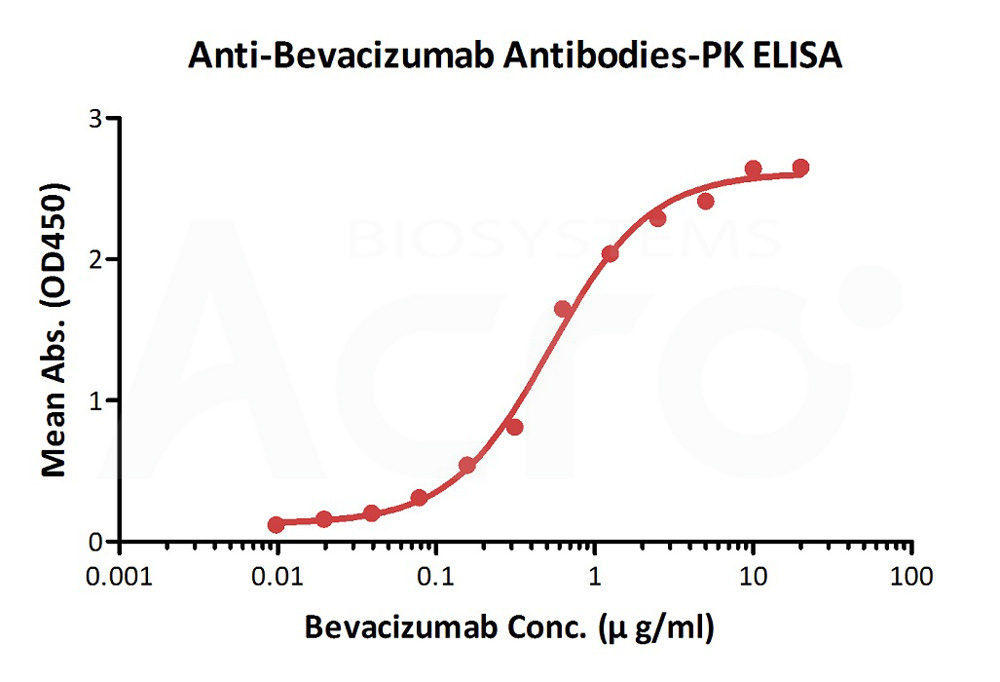
Abstract: Glioblastoma, the most common primary malignant brain tumor in adults, carries a poor prognosis, with a median survival of just 15 months, significantly impacting patients' quality of life. The aggressive growth of these highly vascularized tumors relies heavily on angiogenesis, driven primarily by vascular endothelial growth factor-A. Therefore, VEGF signaling pathway has become a prime therapeutic target in GBM treatment over the past decade. While anti-angiogenic treatment showed promise, agents like bevacizumab have ultimately failed to improve overall survival. This highlights the presence of compensatory angiogenic mechanisms that bypass VEGF inhibition, necessitating further investigation into resistance mechanisms and the development of more effective therapeutic strategies. This review examined the current landscape of anti-angiogenic agents for GBM, analyzed the mechanisms driving resistance to these therapies, and explored potential strategies for enhancing their effectiveness.
Targeted maintenance therapy for a young woman with cervical rhabdomyosarcoma: A case report and review of literatureMa, Zhang, Li
et alWorld J Clin Oncol (2025) 16 (3), 101909
Abstract: Rhabdomyosarcoma of the uterine cervix is a rare form of soft-tissue sarcoma predominantly affecting young women, with no established standard treatment protocol.This report presents a case of a 17-year-old female patient presenting with intermittent, non-cyclical vaginal bleeding and associated lower abdominal pain. Pelvic magnetic resonance imaging and additional examinations led to the diagnosis of cervical rhabdomyosarcoma. The primary treatment options for uterine cervical rhabdomyosarcoma include surgery, with or without adjuvant chemotherapy and radiotherapy. This patient underwent surgery followed by a postoperative chemotherapy regimen of gemcitabine combined with docetaxel and bevacizumab. After 19 months of follow-up, the patient showed no signs of recurrence and maintained good overall health. Given the rarity of cervix rhabdomyosarcoma, this case is presented to provide insights into the diagnosis and treatment of this condition.This suggests that bevacizumab may demonstrate potential efficacy in the treatment of cervical rhabdomyosarcoma. In the future, targeted therapy is expected to play an increasingly significant role in the management of rhabdomyosarcoma.©The Author(s) 2025. Published by Baishideng Publishing Group Inc. All rights reserved.
Predictors of Non-response to Atezolizumab Plus Bevacizumab in Patients With Unresectable Hepatocellular Carcinoma: A Multicentre Real World Study (HCC-AB Study)Singh, Kumar, Kulkarni
et alJ Clin Exp Hepatol (2025) 15 (4), 102513
Abstract: The approved immunotherapies for patients with advanced HCC are Atezolizumab and Bevacizumab. However, patients in India present late and healthcare is often available through self-financing. To rationalise the therapy, we conducted a large multicentre study to identify the baseline predictors of non-response to atezolizumab and bevacizumab in advanced unresectable HCC.A dose of atezolizumab 1200 mg and bevacizumab 15 mg/kg was used every 3 weeks from 6 centres across India. A total of 278 patients were screened, and 160 were included in the study. The study included patients with locally advanced metastatic or inoperable hepatocellular carcinoma who were at least 18 years of age and those who received <3 injections were excluded. Fifty-four percent of the included patients were BCLC-B and 46% were BCLC-C. The primary objective was to study overall survival and progression-free survival. While identifying radiological response, objective response rate and adverse effects were secondary objectives.The mean age was 61.9 ± 11.7 years, 88% were male, 55% had NASH, 16.3% had hepatitis C, 18.8% had hepatitis B and the rest were alcohol. The mean Model for End-Stage Liver Disease (MELD) is 12.05 ± 4.46, Albumin-Bilirubin Score (ALBI) is -2.04 ± 0.57. Fifty-five percent received first-line and 45% as second/other line therapy. The median overall survival was 10 (95% confidence interval [CI]: 6.1-15.6) months. Progression-free survival was found to be 8 (95%CI: 5.1-14.7) months overall. Eleven (6.9%) achieved complete response, 28 (17.5%) partial response, 33 (20.6%) had stable disease and 88 (55%) had progressive disease. On multivariate analysis, CRP>1 mg/dl (P-0.007), PIVKA-II>400 mAU/mL (P-0.019), AFP>100 ng/ml (P-0.009), presence of diabetes (P-0.042) were associated with non-response to atezolizumab and bevacizumab injection. Fifty-three percent of patients developed any grade of adverse effect, and 20% developed grade 3/4 adverse events amounting to the stoppage of therapy.Non-response to atezolizumab and bevacizumab immunotherapy was predicted by CRP>1 mg/dl, PIVKA-II>400mAU/ml, AFP>100 ng/ml and the presence of diabetes.© 2025 Indian National Association for Study of the Liver. Published by Elsevier B.V. All rights are reserved, including those for text and data mining, AI training, and similar technologies.
Unraveling the immune-activated tumor microenvironment correlated with clinical response to atezolizumab plus bevacizumab in advanced HCCLim, Goh, Song
et alJHEP Rep (2025) 7 (4), 101304
Abstract: Despite atezolizumab plus bevacizumab being a standard treatment for advanced hepatocellular carcinoma (HCC), a significant proportion of patients do not achieve durable benefit. This study aimed to identify predictive biomarkers for this therapy by investigating the role of immune activation within the tumor microenvironment (TME).We characterized the intratumoral TME of patients with advanced HCC treated with atezolizumab plus bevacizumab using single cell transcriptomics on pretreatment tumor biopsies from 12 patients. To complement and support these findings, we integrated our single cell data with publicly available bulk RNA-sequencing data from independent clinical trial cohorts.Patients who responded to combination therapy with atezolizumab plus bevacizumab demonstrated an immune-activated TME, marked by enhanced cytotoxicity and a tumor-specific T cell response. These patients also exhibited an increased proportion of inflammatory cytokine-enriched tumor-associated macrophage clusters with stronger interactions with T cells, an increased population of conventional dendritic cells, and activated antigen-presenting function in tumor endothelial cells. When publicly available bulk RNA-sequencing data from independent clinical trial cohorts were analyzed, these immune activation features were associated with improved progression-free survival (median 10.8 months, 95% CI: 7.3-not reached versus 5.5 months, 95% CI: 4.0-6.7; p <0.001).These findings suggest that the existence of an activated immune TME before treatment is crucial for a favorable clinical response in patients with HCC treated with atezolizumab plus bevacizumab.Only a subset of patients with HCC benefit from combination therapy with atezolizumab plus bevacizumab, limiting its clinical utility. In this study, we used single cell RNA analysis to identify TME features associated with a clinical response to this therapy. Our findings suggest that a pre-existing immune-activated TME is crucial for predicting the response to atezolizumab plus bevacizumab. Specifically, features such as enhanced T cell cytotoxicity, inflammatory cytokine-enriched macrophage clusters, active antigen presentation in endothelial cells, and an increased presence of dendritic cells may aid patient selection and inform therapeutic strategies.© 2024 The Authors.















































 膜杰作
膜杰作 Star Staining
Star Staining