Erythromycin repurposing for hepatocellular carcinoma treatment: Targeting CD24 to enhance anti-tumor immunityShao, Zhao, Qian
et alEur J Pharmacol (2025) 998, 177457
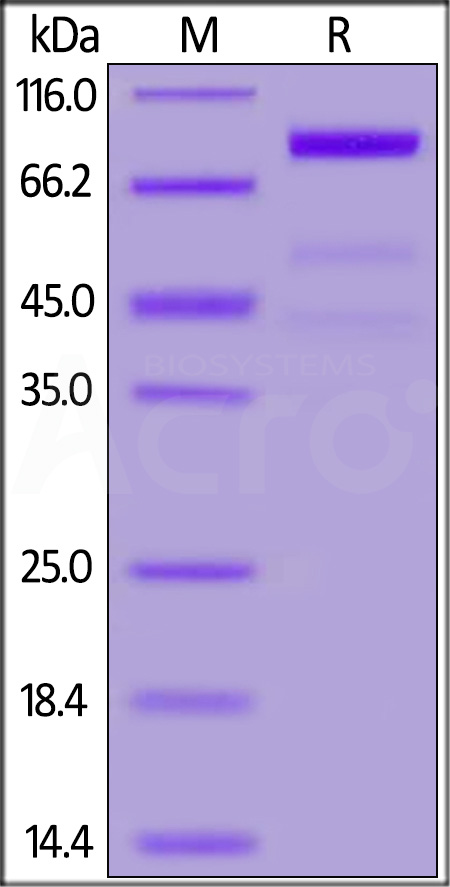
Abstract: Hepatocellular carcinoma (HCC) is a malignant tumor, making up about 90% of all primary liver cancers and ranking as a top cause of cancer mortality globally. With the severe side effects of conventional radiotherapy and chemotherapy, there's an ongoing quest for less toxic treatment options. CD24, a highly glycosylated membrane surface protein, plays a role in cancer cell adhesion and metastasis. Its overexpression is associated with poor prognosis in cancer patients. By binding to Siglec-10 on macrophages, CD24 helps tumor cells dodge the immune system. Targeting CD24 expression on is seen as a promising approach to cancer therapy. This study investigated the potential of repurposing the old drug erythromycin to regulate CD24 and its anti-HCC effect. The results investigated that erythromycin didn't significantly impact liver cancer cell growth, movement, or death. However, it effectively inhibited CD24 expression after treatment, and the effect that can be reversed with a proteasome inhibitor MG132. Further study showed erythromycin not only reduced CD24 expression but also slowed tumor growth, triggered cell death, and altered the balance of proteins involved in cell proliferation and migration in vivo. Importantly, it altered the immune environment within tumors and boosted the presence of immune cells that fight cancer including the infiltration increase of M1 macrophages and T lymphocytes in tumor tissues and the decrease of M2 macrophages. The research confirmed that erythromycin enhanced the anti-tumor immune response in HCC-bearing mice by reducing CD24 expression, providing a novel strategy for the clinical development of HCC treatments.Copyright © 2025 Elsevier B.V. All rights reserved.
The molecular basis of immunosuppression by soluble CD52 is defined by interactions of N-linked and O-linked glycans with HMGB1 box BDeBono, D'Andrea, Bandala-Sanchez
et alJ Biol Chem (2025) 301 (4), 108350
Abstract: Human soluble CD52 is a short glycopeptide comprising 12 amino acids (GQNDTSQTSSPS) which functions as an immune regulator by sequestering the pro-inflammatory high mobility group box protein 1 (HMGB1) and suppressing immune responses. Recombinant CD52 has been shown to act as a broad anti-inflammatory agent, dampening both adaptive and innate immune responses. This short glycopeptide is heavily glycosylated, with a complex sialylated N-linked glycan at N3 and reported O-linked glycosylation possible on several serine and threonine residues. Previously we demonstrated that specific glycosylation features of CD52 are essential for its immunosuppressive function, with terminal α-2,3-linked sialic acids required for binding to the inhibitory SIGLEC-10 receptor leading to T-cell suppression. Using high resolution mass spectrometry, we have further characterized the N- and O-linked glycosylation of Expi293 recombinantly produced CD52 at a glycopeptide and released glycan level, accurately determining glycan heterogeneity of both N- and O-linked glycosylation, and localizing the site of O-glycosylation to T8 with high confidence and direct spectral evidence. This detailed knowledge of CD52 glycosylation informed the construction of a model system, which we analyzed by molecular dynamics simulations to understand the mechanism of recognition and define interactions between bioactive CD52, HMGB1 and the SIGLEC-10 receptor. Our results confirm the essential role of glycosylation, more specifically hyper-sialylation, in the function of CD52, and identify at the atomistic level specific interactions between CD52 glycans and the Box B domain of HMGB1 that determine recognition, and the stability of the CD52/HMGB1 complex. These insights will inform the development of synthetic CD52 as an immunotherapeutic agent.Copyright © 2025 The Authors. Published by Elsevier Inc. All rights reserved.
CD24-Fc resolves inflammation and rescues CD8 T cells with polyfunctionality in humanized mice infected with HIV-1 under cARTLi, Ma, Yu
et albioRxiv (2024)
Abstract: The persistence of HIV-1 reservoirs during combination anti-retroviral therapy (cART) leads to chronic immune activation and systemic inflammation in people with HIV (PWH), associating with a suboptimal immune reconstitution as well as an increased risk of non-AIDS events. This highlights the needs to develop novel therapy for HIV-1 related diseases in PWH. In this study, we assessed the therapeutic effect of CD24-Fc, a fusion protein with anti-inflammatory properties that interacts with danger-associated molecular patterns (DAMPs) and siglec-10, in chronic HIV-1 infection model using humanized mice undergoing suppressive cART. Our findings show that CD24-Fc treatment significantly reduced inflammation and immune hyperactivation in vivo when combined with cART. CD24-Fc mediated resolution of inflammation was associated with improved recovery of CD4 T cells, reduced immune activation, restored central memory T cells and reversal of immune cell exhaustion phenotype. Notably, CD24-Fc treatment rescued CXCR5+ CD8 central memory T cell (TCM) which correlated with increased polyfunctionality in HIV-specific T cells in humanized mice and in cultured peripheral blood mononuclear cells (PBMCs) from PWH. This restoration of CXCR5+ memory CD8 T cells was associated with HIV replication inhibition, delayed viral rebound and reduced HIV-1 pathogenesis upon cART cessation. This study suggests that CD24-Fc treatment could represent a promising new therapeutic strategy for managing chronic systemic inflammation and associated diseases in PWH.
Soluble CD52 mediates immune suppression by human seminal fluidHarrison, Stone, Bandala-Sanchez
et alFront Immunol (2024) 15, 1497889
Abstract: Seminal fluid provides for the carriage and nutrition of sperm, but also modulates immunity to prevent allo-rejection of sperm by the female. Immune suppression by seminal fluid has been associated with extracellular vesicles, originally termed prostasomes, which contain CD52, a glycosylated glycophosphoinositol-anchored peptide released from testicular epithelial cells. Previously, we reported that human T cell-derived CD52, bound to the danger-associated molecular pattern protein, high mobility group box 1 (HMGB1), suppresses T cell function via the inhibitory sialic acid-binding immunoglobulin-like lectin-10 (Siglec-10) receptor. Here we show that human seminal fluid contains high concentrations of CD52 complexed with HMGB1, which mediates T cell suppression indirectly via Siglec-7 on antigen-presenting cells. Proliferation of natural killer (NK) cells, which express Siglec-7 and play a key role in the immune defence of the uterus, was directly suppressed by seminal fluid CD52. These findings elucidate a critical function of seminal fluid to suppress cellular immunity and facilitate reproduction.Copyright © 2024 Harrison, Stone, Bandala-Sanchez, Huntington, McLachlan, Rautela and O’Bryan.
 +添加评论
+添加评论























































 膜杰作
膜杰作 Star Staining
Star Staining
















