Halofuginone Disrupted Collagen Deposition via mTOR-eIF2α-ATF4 Axis to Enhance Chemosensitivity in Ovarian CancerLi, Wu, Zhang
et alAdv Sci (Weinh) (2025)
Abstract: The interplay between cancer-associated fibroblasts (CAFs) and extracellular matrix (ECM) mediates progress, metastasis, and therapy resistance. However, strategy of targeting ECM remodeling to enhance chemosensitivity in ovarian cancer remains elusive. Here, a 22-gene matrisome signature predicts chemotherapy response and survival in ovarian cancer. The dense, collagen-rich ECM secreted by CAFs harbors more M2 tumor-associated macrophages (TAMs) than the looser ECM based on single cell RNA-seq (scRNA-seq) of ovarian cancer, suggesting the promising approach of targeting collagen to remodel ECM. An integrated analysis identifies collagen type I alpha 1 chain (COL1A1) as a major component of the ECM that contributes to chemoresistance and poor prognosis, highlighting its potential as a therapeutic target. Halofuginone (HF), a clinically active derivative of febrifugine, is identified as a COL1A1-targeting natural compound by screening the Encyclopedia of Traditional Chinese Medicine (ETCM). Mechanistically, HF inhibits COL1A1 production via the mTOR-eIF2α-ATF4 axis in CAFs. Notably, HF disrupts collagen deposition and promotes CD8+ T cell infiltration, partially via M2-M1 macrophage polarization to enhance chemosensitivity. Overall, the findings suggest that HF combined with chemotherapy is a promising and effective treatment for ovarian cancer.© 2025 The Author(s). Advanced Science published by Wiley‐VCH GmbH.
A parainfluenza virus 5 (PIV5)-vectored intranasal SARS-CoV-2 vaccine (CVXGA1) elicits protective and long-lasting immunity in nonhuman primatesBeavis, Xiao, Gingerich
et alJ Virol (2025)
Abstract: Waning immunity from approved COVID-19 vaccines and emerging variants of SARS-CoV-2 necessitate the need to develop alternative COVID-19 vaccines for improved durability and broader protection. This work investigates the efficacy and mucosal, humoral, and cellular immunogenicity of intranasal, parainfluenza virus 5 (PIV5)-vectored COVID-19 vaccine CVXGA1 in an African green monkey (AGM) nonhuman primate model. A single intranasal dose of CVXGA1 induced robust and sustained humoral and cellular immune responses in AGMs and protected against SARS-CoV-2 ancestral WA1 strain and alpha variant challenge infection in the respiratory tracts as demonstrated by lack of viral load and greatly decreased histopathology. Mucosal IgA antibodies were detected in the upper and lower respiratory tracts of immunized AGMs. CVXGA1-vaccinated AGMs maintained serum anti-S IgG and IgA antibody titers for over 245 days. S-specific CD4+ and CD8+ T cells producing predominantly IFN-γ, TNF-α, MIP-β, and CD107α cytokines peaked on day 28 and could be detected on day 180 by intracellular cytokine staining of peripheral blood mononuclear cells (PBMC). IL13-secreting CD4+ and CD8+ T cells were minimally detected, indicative of a dominant type 1 immune response. These data supported the clinical evaluation of CVXGA1 intranasal COVID-19 vaccine. These data demonstrate that intranasal immunization with CVXGA1 induces long-lasting protective SARS-CoV-2 S-specific mucosal, humoral, and cellular responses in AGMs.IMPORTANCEThe continued threat of SARS-CoV-2 indicates the need for a novel vaccine that induces long-lasting mucosal, cellular, and humoral immunity, as well as block transmission. This work demonstrates that intranasal, PIV5 viral-vectored SARS-CoV-2 vaccine CVXGA1 induces mucosal immunity and long-lasting cellular and humoral immunity that protects African green monkeys from SARS-CoV-2 challenge. The ability of our intranasal vaccine to elicit long-lasting mucosal, cellular, and humoral immunity against SARS-CoV-2 indicates great promise of the PIV5-vectored COVID-19 vaccine for further clinical development.
Upregulation of RIG-I is Critical for Responsiveness to IFN-α Plus Anti-PD-1 in Colorectal CancerNie, Fang, Zhou
et alCancer Med (2025) 14 (6), e70802
Abstract: Immunotherapy is a promising and effective approach that has achieved significant curative effects in colorectal cancer (CRC). Recently, retinoic acid-inducible gene I (RIG-I) has been shown to play a critical role in tumor immunity. However, the correlation between RIG-I and immunotherapy in CRC remains unclear.RIG-I expression was measured in CRC and normal samples based on analysis of the public databases, a tissue microarray, and CRC cell lines. The correlation between RIG-I and immune microenvironment was explored using well-established biological algorithms and in vitro and in vivo experiments.We discovered that RIG-I expression was downregulated in CRC compared with normal samples. The bioinformatic algorithms indicated that high RIG-I-expressing samples showed a positive correlation with IFN-α response and enrichment of antitumor immune cells, especially CD8+ T cells. Furthermore, knockdown of RIG-I expression efficiently reduced the cell death, STAT1 phosphorylation, and CXCL10/11 expression induced by IFN-α in CRC cells. Finally, an in vivo study showed that the infiltration of CD3+ CD8+ T cells was significantly decreased in the RIG-I knockout group. An animal model further confirmed that the inhibition of tumor growth induced by IFN-α plus anti-PD-1 therapy was dependent on RIG-I expression.RIG-I is a promising biomarker for CRC immunotherapy, which provides a novel concept for combinatorial immunotherapy.© 2025 The Author(s). Cancer Medicine published by John Wiley & Sons Ltd.
Preventive effects of low-dose radiation and hypofractionated radiation plus anti-programmed cell death protein 1 on lung metastasis in breast cancerChen, Deng, He
et alOncol Res (2025) 33 (3), 687-694
Abstract: Previous experiments have demonstrated that hypofractionated radiation therapy (HFRT), low-dose radiation therapy (LDRT), and combined anti-programmed cell death protein 1 (αPD-1) can enhance the abscopal effect. Combined with the phenomenon of low prognosis in patients with breast cancer lung metastasis, our study establishes a mouse model and changes the irradiation regimen of LDRT to explore its preventive effect on breast cancer lung metastasis.The breast cancer subcutaneous graft tumor model was developed. Two-lung prophylactic LDRT was performed prior to the onset of lung metastases, in combination with HFRT (8 Gy, 3f), and αPD-1 (200 μg, 4f) therapy. We watched and documented the tumor volume, survival duration, and number of lung metastases. Furthermore, after labeling the corresponding cells using markers, we detected immune-related cell infiltration by immunohistochemistry and flow cytometry, such as T cells. We also determined the expression of cytokines (IFN-γ and TNF-α) by enzyme-linked immunosorbent assay.The triple therapy (HFRT+LDRT+αPD-1) resulted in tumor shrinkage and prolonged survival in mice, with median survival extending from 35 to 52 days. The most notable decrease in the quantity of advanced lung metastatic nodules in breast cancer was observed with the triple therapy (HFRT+LDRT+αPD-1) (p < 0.05). Furthermore, according to immunohistochemistry and flow cytometry, the triple treatment (HFRT+LDRT+αPD-1) showed the greatest expression of CD8+ T cells. Additionally, the ratio of CD8+/CD4+ T cells was considerably greater than that of the groups (p < 0.0001). Triple therapy (HFRT+LDRT+αPD-1) increased the recruitment of DCs cells, promoted IFN-γ and TNF-α expression, and curbed the aggregation of MDSCs cells (p < 0.05).Prophylactic LDRT to the lungs, based on HFRT and αPD-1, can enhance anti-tumor efficacy and prevent advanced lung metastases from breast cancer. The process involves boosting the recruitment of DCs and CD8+ T cells, preventing MDSC cell aggregation, and lessening the tumor microenvironment's immunosuppressive effects.© 2025 The Author.

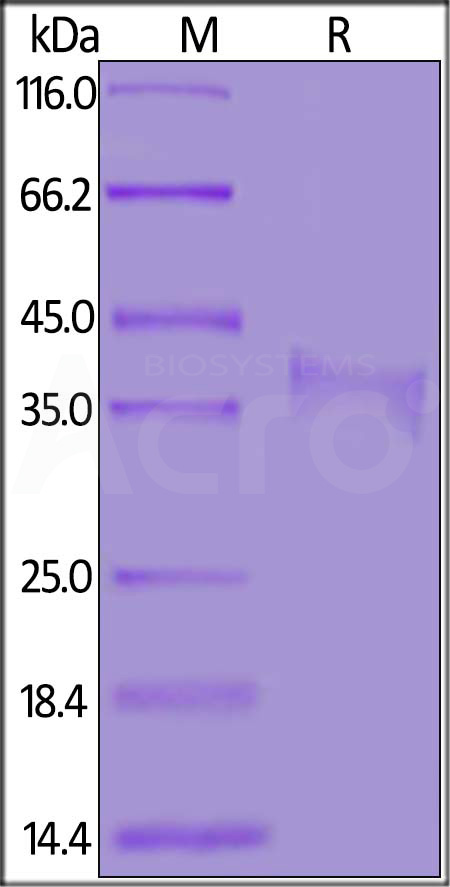























































 膜杰作
膜杰作 Star Staining
Star Staining















