Aqueous humor mediator levels as biomarkers of anti-VEGF response in age-related macular degenerationBaillif, Nahon-Esteve, Pace-Loscos
et alCytokine (2025) 190, 156921
Abstract: To monitor intraocular mediator dynamics in treatment-naïve neovascular age-related macular degeneration (nAMD) patients treated with anti-VEGF intravitreal injections (IVIs) to identify individual mediator patterns correlating with treatment response.Interventional, monocentric, prospective, clinical study.Treatment-naïve nAMD patients.Aqueous humor samples (100-200 μL) were collected by clear cornea paracentesis at baseline (before the first anti-VEGF IVI) and before the second and third anti-VEGF IVIs. The levels of 13 intraocular mediators were measured (VEGF-A, VEGF-C, PlGF, IL-1β, IL-6, IL-10, IL-18, CXCL1, CXCL5, CXCL7, CXCL8, MIP-1α and TNFα) using multiplex arrays.The primary endpoint was the changes in intraocular inflammatory mediator levels between baseline and month 3. Secondary endpoints were the changes in best-corrected visual acuity (BCVA) and Central Retinal Thickness (CRT) between baseline and month 4.Fifteen eyes were included in the study. BCVA remained stable throughout the study (p = 0.07). CRT, foveal thickness, and the presence of intraretinal and subretinal fluid significantly decreased after anti-VEGF IVIs (p < 0.0001, p < 0.0001, p < 0.001 and p < 0.001, respectively). After anti-VEGF IVIs, VEGF-A levels significantly decreased (p < 0.0001). No significant differences in all other mediator levels were observed. Three patients had baseline VEGF-A levels ≤50 pg/mL: they showed higher baseline IL-6 levels (p = 0.05), and elevated IL-6 (p = 0.03), PlGF (p = 0.02), VEGF-C (p = 0.005), IL-8 (p = 0.04), and TNFα (p = 0.013) levels after the first IVI. Good clinical responders had significantly higher baseline VEGF-A levels (p = 0.007). Patients who required a fourth IVI within 8 weeks of the loading dose had higher baseline TNFα levels (p = 0.05); higher MIP-1α levels after the first IVI (p = 0.045); and elevated TNFα (p = 0.026) and IL-8 (p = 0.029) levels after the second IVI.The aqueous humor levels of the studied mediators remained stable after anti-VEGF IVIs, except for a significant decrease in VEGF-A levels in all patients. Patients with low baseline intraocular VEGF-A levels (i.e., ≤50 pg/mL) showed an intraocular inflammatory profile with elevated IL-6, PlGF, VEGF-C, IL-8 and TNFα levels. Treatment response correlated with high baseline VEGF-A levels. An interval > 8 weeks between the third and fourth anti-VEGF IVIs was associated with a pro-angiogenic/pro-inflammatory environment.Copyright © 2025. Published by Elsevier Ltd.
The Genetic and Biological Basis of Pseudoarthrosis in Fractures: Current Understanding and Future DirectionsKotsifaki, Kalouda, Maroulaki
et alDiseases (2025) 13 (3)
Abstract: Pseudoarthrosis-the failure of normal fracture healing-remains a significant orthopedic challenge affecting approximately 10-15% of long bone fractures, and is associated with significant pain, prolonged disability, and repeated surgical interventions. Despite extensive research into the pathophysiological mechanisms of bone healing, diagnostic approaches remain reliant on clinical findings and radiographic evaluations, with little innovation in tools to predict or diagnose non-union. The present review evaluates the current understanding of the genetic and biological basis of pseudoarthrosis and highlights future research directions. Recent studies have highlighted the potential of specific molecules and genetic markers to serve as predictors of unsuccessful fracture healing. Alterations in mesenchymal stromal cell (MSC) function, including diminished osteogenic potential and increased cellular senescence, are central to pseudoarthrosis pathogenesis. Molecular analyses reveal suppressed bone morphogenetic protein (BMP) signaling and elevated levels of its inhibitors, such as Noggin and Gremlin, which impair bone regeneration. Genetic studies have uncovered polymorphisms in BMP, matrix metalloproteinase (MMP), and Wnt signaling pathways, suggesting a genetic predisposition to non-union. Additionally, the biological differences between atrophic and hypertrophic pseudoarthrosis, including variations in vascularity and inflammatory responses, emphasize the need for targeted approaches to management. Emerging biomarkers, such as circulating microRNAs (miRNAs), cytokine profiles, blood-derived MSCs, and other markers (B7-1 and PlGF-1), have the potential to contribute to early detection of at-risk patients and personalized therapeutic approaches. Advancing our understanding of the genetic and biological underpinnings of pseudoarthrosis is essential for the development of innovative diagnostic tools and therapeutic strategies.
sFlt-1/PlGF ratio combined with endocan-1 serum levels improves the predictive values for the occurrence and prognosis of preeclampsia in a single centre studyTian, He, Pan
et alJ Hum Hypertens (2025)
Abstract: This retrospective study evaluated diagnostic and prognostic values of sFlt-1/PlGF ratio combined with serum endocan-1 for preeclampsia (PE). This study included 105 patients with PE admitted at Xiamen University Affiliated Xiang'an Hospital from January 2020 to September 2023, with 90 healthy pregnant women receiving routine check-ups during the same period as controls. sFlt-1, PlGF, and endocan-1 levels were measured, and sFlt-1/PlGF ratio was calculated. The correlation of sFlt-1/PlGF ratio with serum endocan-1 levels was analysed, and influencing factors for poor prognosis of PE patients were screened. Diagnostic and prognostic values of sFlt-1/PlGF ratio combined with serum endocan-1 were assessed. Results showed an increase in sFlt-1/PlGF ratio and serum endocan-1 levels in PE patients and a positive correlation between them. For assisting in the diagnosis of PE, the AUC of the sFlt-1/PlGF ratio combined with serum endocan-1 was 0.874 (95%CI: 0.819 - 0.917; sensitivity, 75.24%; specificity, 100.00%), which was superior over that of sFlt-1/PlGF ratio (P = 0.025) and endocan-1 (P = 0.047) alone. Elevated sFlt-1/PlGF ratio and serum endocan-1 levels were independent risk factors for poor prognosis of PE patients. For assisting in predicting poor prognosis of PE, the AUC of sFlt-1/PlGF ratio with serum endocan-1 was 0.955 (95%CI: 0.896 - 0.986; sensitivity, 82.61%; specificity, 100.00%), which was higher than that of sFlt-1/PlGF ratio (P = 0.023) or serum endocan-1 (P = 0.010) alone. Altogether, sFlt-1/PlGF ratio combined with serum endocan-1 is advantageous over sFlt-1/PlGF ratio and serum endocan-1 alone for predicting PE occurrence and prognosis.© 2025. The Author(s), under exclusive licence to Springer Nature Limited.
First trimester placental growth factor and uterine artery pulsatility index in the prediction of preeclampsia in high-risk pregnancyHodžić, Muračević, Gračić
et alMed Glas (Zenica) (2025) 22 (1), 71-77
Abstract: To identify the most effective screening method for preeclampsia by evaluating the predictive significance of measuring serum placental growth factor (PlGF) concentration and using Doppler ultrasound assessments of uterine artery blood flow during the first trimester in high-risk pregnancies as predictors of preeclampsia.A prospective screening study involving 173 high-risk pregnant women for preeclampsia, between 11 + 0 and 13 + 6 weeks of gestation was conducted. Women were divided into two groups based on pregnancy outcome: a control group of 158 pregnant women who remained normotensive, and a group of 15 high-risk pregnant women who developed symptoms of preeclampsia during pregnancy. Serum PlGF concentration using a quantitative enzyme-linked immunosorbent assay was determined.PlGF level was significantly reduced in women who later developed preeclampsia (14.06 pg/mL) compared to controls (37.46 pg/mL). The uterine artery pulsatility index (UtA-PI) was significantly increased in the preeclamptic group (1.73) compared to the control group (1.44). For screening preeclampsia using the combination of PlGF and UtA-PI, the estimated detection rates were 66.67% at the fixed false-positive rate (FPR) of 5% and 73.33% at the FPR of 10%. The best screening results were obtained using regression models including maternal characteristics PlGF, and UtA-PI, yielding estimated detection rates of 73.33% at the FPR of 5% and 86.67% at the FPR of 10%, respectively.Placental growth factor level, in conjunction with uterine artery pulsatility index during the first trimester was a valuable and accurate biomarker for predicting preeclampsia in high-risk pregnancies. When integrated with comprehensive medical history, these markers enhance the assessment of preeclampsia risk.Copyright© by the Medical Assotiation of Zenica-Doboj Canton.

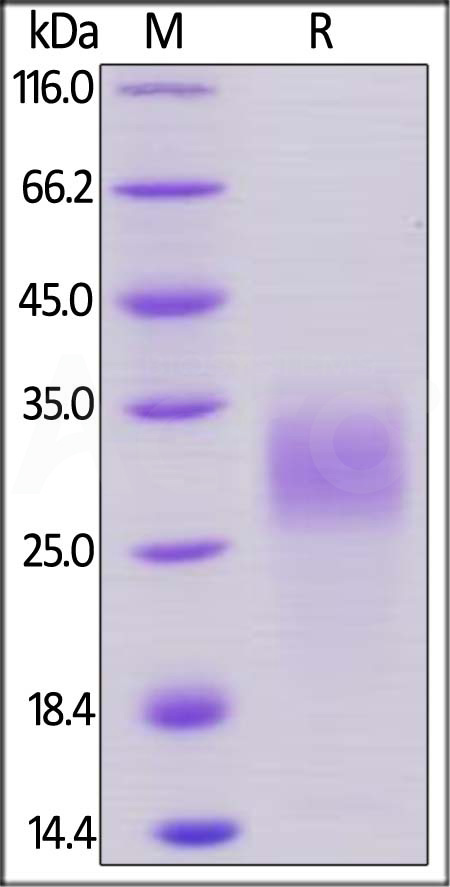
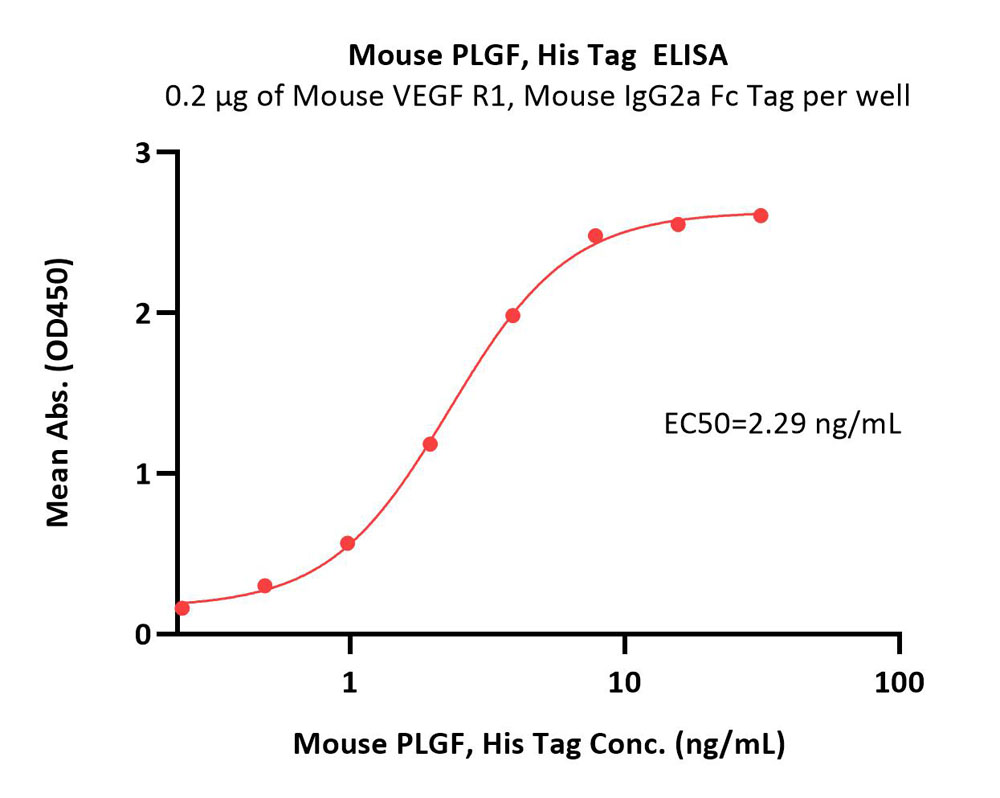















































 膜杰作
膜杰作 Star Staining
Star Staining