Emerging roles of SLAMF7 in immune cells and related diseasesZhang, Zhang, Chen
et alInnate Immun (2025) 31, 17534259251326700
Abstract: Immune cells are heterogeneous and perform different functions in different microenvironment, thus playing different roles in different stages of diseases. Studies have shown that immune cells are involved in the pathogenesis of many diseases, and there is a causal association of immune cells with disease states. Signaling Lymphocyte Activation Molecule family (SLAMF) members are a newly appreciated group of specific receptors that are mainly expressed in immune cells and whose role is to regulate the function of immune cells. SLAMF7, also known as CD319, has been widely reported in multiple myeloma, and in recent years, more and more studies have shown that SLAMF7 is widely involved in the function of immune cells and the progression of breast cancer, acquired immune deficiency syndrome, systemic lupus erythematosus and other immune cells-related diseases. However, the mechanisms underlying the regulatory role of SLAMF7 on immune cells, and the impact on the progression of immune cells-related diseases remain poorly elucidated. In this review, we summarize current knowledge about the role of SLAMF7 in immune cells and related diseases such as cancer, infectious disease, autoimmune disease and atherosclerosis, and the therapeutic strategy targeting SLAMF7 is also described. By better understanding the role and regulation of SLAMF7, we hope to provide new insights and directions for improving the diagnosis and treatment of inflammation.
How First-Line Therapy is Changing in Transplant-Eligible Multiple Myeloma PatientsHoubaida, Del Giudice, Galimberti
et alMediterr J Hematol Infect Dis (2025) 17 (1), e2025026
Abstract: Multiple myeloma is a malignant haematological neoplasm characterised by the proliferation of plasma cells in the bone marrow. Each year, over 35,000 new cases are diagnosed in the United States, and nearly 13,000 patients die from the disease.1 The main cause of morbidity is bone disease, characterised by osteolytic lesions, which, unlike other malignancies that metastasise to bone, are not followed by new bone formation.2 Other major clinical manifestations include anaemia, hypercalcemia, renal failure, and an increased risk of infections. Approximately 1-2% of patients present with extramedullary disease (EMD) at the time of diagnosis, while 8% develop EMD later in the course of the disease.3 Although multiple myeloma remains incurable, its treatment continues to evolve rapidly. Approved therapies include immunomodulatory agents (IMiDs, such as thalidomide, lenalidomide, and pomalidomide), proteasome inhibitors (bortezomib, carfilzomib, and ixazomib), and monoclonal antibodies (mAb) targeting CD38 (especially daratumumab and isatuximab) and SLAMF7. New therapeutic avenues include bispecific antibodies and chimeric antigen receptor T-cell (CAR-T) therapy.4-5 The latest ESMO (European Society for Medical Oncology)6 and NCCN (National Comprehensive Cancer Network) guidelines7 have set the standard of care for patients with newly diagnosed multiple myeloma (NDMM) eligible for transplantation, particularly those in good general condition and < 70 years old. This approach is divided into four phases: induction therapy, hematopoietic stem cell collection, and autologous transplant, consolidation, and maintenance. The most significant differences between the guidelines occur during the induction phase, influenced by regulatory approvals in the United States and Europe. This article will focus on the changing landscape of therapies for newly diagnosed multiple myeloma (NDMM) in transplant-eligible.
The multifaceted role of CS1 (SLAMF7) in immunoregulation: Implications for cancer therapy and autoimmune disordersAltalbawy, Babamuradova, Baldaniya
et alExp Cell Res (2025) 447 (1), 114516
Abstract: CS1 (SLAMF7), a pivotal immune receptor, plays a dual role in modulating immune responses in autoimmune diseases and cancer. In autoimmunity, aberrant CS1 signaling contributes to the activation of autoreactive lymphocytes, driving pathologies such as systemic lupus erythematosus (SLE) and rheumatoid arthritis (RA). Conversely, in oncology, CS1 serves as a promising immunotherapeutic target, exemplified by the efficacy of the monoclonal antibody Elotuzumab in multiple myeloma. CS1 mediates immune cell functions through intricate signaling pathways, including interactions with EAT-2 and SAP adaptors, which influence cytotoxicity, cytokine production, and immune homeostasis. Beyond cancer and autoimmune diseases, soluble and membrane-bound forms of CS1 are emerging as biomarkers and potential therapeutic targets. Despite significant progress, gaps remain in understanding CS1\u2019s mechanisms, variability in expression, and role in other diseases. This study explores the multifaceted functions of CS1, proposing innovative strategies to leverage its therapeutic potential across diverse pathologies.Copyright © 2025 Elsevier Inc. All rights reserved.
Memory-like NK cell differentiation, inhibitory NKG2A blockade, and improved recognition via antibody or CAR engineering combine to enhance NK cell attack against multiple myelomaZhou, Marin, Afrin
et alJ Immunol (2025) 214 (1), 1-11
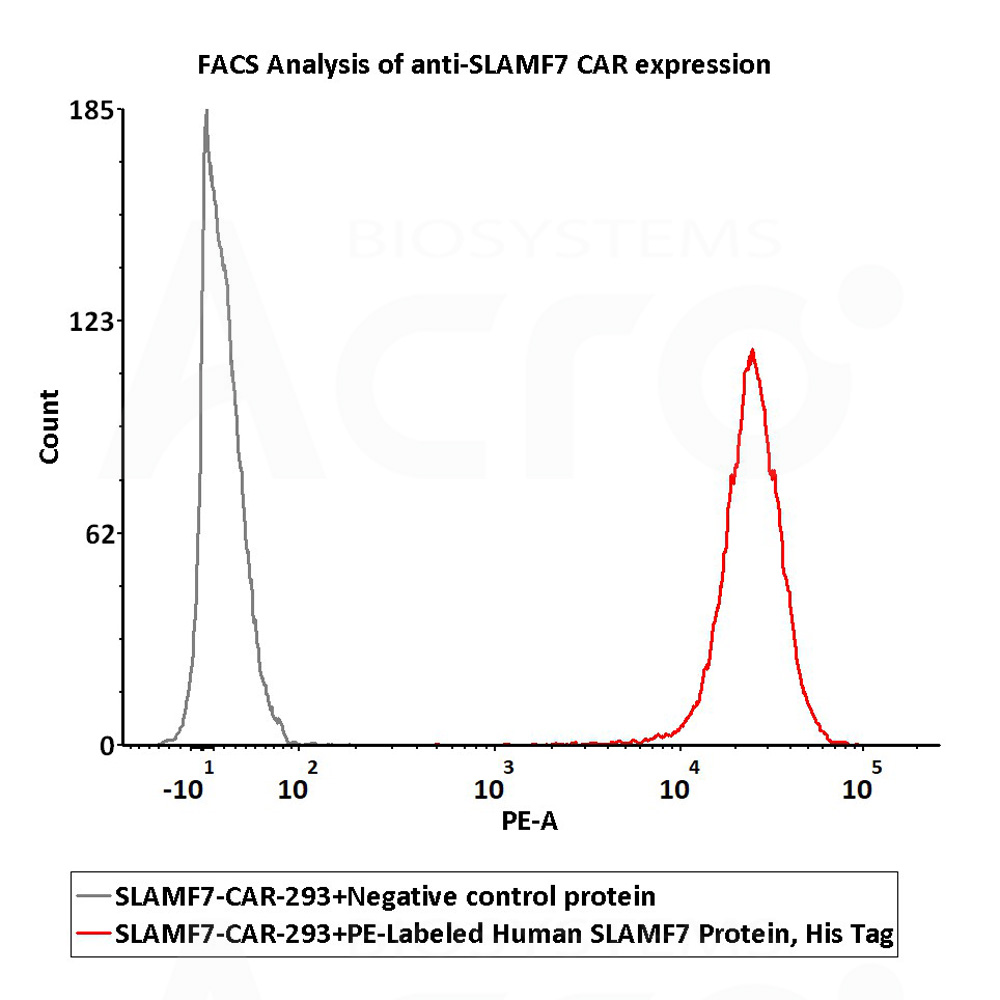
Abstract: Natural killer (NK) cells are a promising approach for cellular cancer immunotherapy and are being investigated to treat patients with multiple myeloma (MM). We found that MM patient blood NK cell frequencies were normal with increased activating receptors and cytotoxic granules, without evidence of functional exhaustion. Despite this activated state, MM target cells were resistant to conventional NK cells by unclear mechanisms. Memory-like (ML) NK cells are generated after brief activation via the interleukin (IL)-12, IL-15, and IL-18 receptors and exhibit multiple enhanced antitumor properties. ML NK cell differentiation improved healthy donor and MM patient NK cell responses against MM target cells, in vitro and in vivo in immunodeficient murine xenograft models. Moreover, incorporating NKG2A checkpoint blockade to overcome HLA-E-induced inhibition further enhanced ML NK cell responses against MM in vitro and in vivo. Because activating receptor recognition of MM by ML NK cells was inadequate, strategies to improve this were investigated. Utilizing anti-SLAMF7 monoclonal antibody (elotuzumab) or anti-BCMA chimeric antigen receptors resulted in robust increases in ML NK cell functional responses against MM. In summary, ML differentiation enhances NK cell attack against myeloma, and combination with approaches to block inhibitory checkpoints and promote MM-specific activation are promising translational NK cell strategies for MM immunotherapy.© The Author(s) 2025. Published by Oxford University Press on behalf of The American Association of Immunologists. All rights reserved. For commercial re-use, please contact reprints@oup.com for reprints and translation rights for reprints. All other permissions can be obtained through our RightsLink service via the Permissions link on the article page on our site—for further information please contact journals.permissions@oup.com.























































 膜杰作
膜杰作 Star Staining
Star Staining
















