Baicalein Ameliorates Experimental Ulcerative Colitis Recurrency by Downregulating Neonatal Fc Receptor via the NF-κB Signaling PathwayHu, Lu, Guan
et alACS Omega (2025) 10 (10), 10701-10712
Abstract: Ulcerative colitis (UC) is a chronic autoimmune disease (AID) that causes mild to moderate unpredictable symptoms, including diarrhea and abdominal pain. Against neonatal Fc receptor (FcRn) has been proven to be a unique AID treatment strategy by decreasing the effects of pathogenic autoantibody. Our previous study revealed that FcRn inhibition is beneficial in UC treatment through reducing colonic neutrophil extracellular trap (NET) formation via accelerating serum antineutrophil cytoplasm antibodies (ANCA) clearance. In this study, we initially confirmed the specific impact of downregulating FcRn in preventing UC relapse by injecting rAAV, which is carrying Fcgrt-shRNA, in mice. Next, we investigated the inhibition effects and regulation mechanisms of baicalein (BCL) on FcRn and assessed its capacity to withstand UC recurrence using NCM460 cells and dextran sodium sulfate-induced mice models by determining the expression of FcRn and its related transcription factors. We also measured colonic NET-associated protein (NAP) expression and serum concentrations of IgG, ANCA, TNF-α, IL-1β, and c-reactive protein (CRP). UC inflammation severity was determined by using the disease activity index (DAI) and histopathological score (HS). BCL treatment remarkably decreased the mRNA and protein contents of FcRn, p50, and p65 but did not impact STAT1 expression or the phosphorylation of IκB and STAT1. Long-term BCL administration inhibited colonic FcRn expression and reduced serum ANCA levels, colonic NAP expression, serum inflammation-related indexes (including TNF-α, IL-1β, and CRP), and DAI and HS scores in UC mice during inflammation relapse better than salazosulfapyridine. Our study indicates that BCL ameliorates UC recurrency by inhibiting FcRn expression via p50/p65 heterodimer-mediated NF-κB signaling.© 2025 The Authors. Published by American Chemical Society.
Pharmacodynamics, pharmacokinetics, and toxicology of Fc-growth hormone fusion protein in macaquesLiu, Peng, Zhou
et alGrowth Horm IGF Res (2025) 81, 101648
Abstract: Growth hormone (GH) therapy for GH deficiency is used to treat multiple conditions. However, the short half-life of GH necessitates frequent dosing, which limits patient adherence. Fc fusion proteins, created by binding an active peptide to the Fc portion of IgG, are known to prolong the plasma half-life of the peptide. Pharmacodynamics and pharmacokinetics of Fc-GH in rats have been reported; however, studies in primate models are lacking. Therefore, in this study, we aimed to investigate the pharmacodynamics, pharmacokinetics, and toxicology of Fc-GH in rhesus and crab-eating macaques.In rhesus macaques, Fc-GH was injected subcutaneously at 0.8, 1.6, and 3.2 mg/kg and intravenously at 1.6 mg/kg. The 1.6 mg/kg subcutaneous dose was administered five times, once every 7 days; other doses were administered as single injections for pharmacodynamic and pharmacokinetic assessments. In crab-eating macaques, potential toxicity was evaluated after single subcutaneous injections at 30, 45, and 62.5 mg/kg and repeated injections at 3, 10, and 30 mg/kg once every 7 days, followed by an 8-week recovery.No adverse events were observed following Fc-GH administrations. Fc-GH achieved Cmax slowly after subcutaneous administration and rapidly after intravenous administration, with plasma levels being maintained over time. In rhesus macaques, the half-life increased dose-dependently: 23.72 ± 2.17 h (0.8 mg/kg), 49.44 ± 14.77 h (1.6 mg/kg), and 76.07 ± 13.19 h (3.2 mg/kg). After five injections of 1.6 mg/kg, the half-life of Fc-GH was 60.42 ± 18.29 h. Insulin-like growth factor 1 (IGF-1) and insulin-like growth factor binding protein 3 (IGFBP-3) levels significantly increased and remained elevated for 28-42 days after Fc-GH injections. In crab-eating macaques, no Fc-GH accumulation was observed. The maximum tolerated single subcutaneous dose was 62.5 mg/kg; no adverse effects were observed at 30 mg/kg during repeated administration over 29 injections with an 8-week recovery.Fc-GH demonstrated favorable pharmacokinetics and pharmacodynamics in macaques, significantly extending the half-life and enhancing IGF-1 and IGFBP-3 levels without adverse effects. These findings suggest Fc-GH as a promising long-acting GH therapy that could improve patient adherence.Copyright © 2025 Elsevier Ltd. All rights reserved.
Role of Antibody Glycosylation in Health, Disease, and TherapyNimmerjahn
Handb Exp Pharmacol (2025)
Abstract: Immunoglobulin G (IgG) antibodies are an essential component of humoral immunity protecting the host from recurrent infections. Among all antibody isotypes, IgG antibodies have a uniquely long half-life, can basically reach any tissue in the body, and have the ability to kill opsonized target cells, which has made them the molecule of choice for therapeutic interventions in cancer and autoimmunity. Moreover, IgG antibodies in the form of pooled serum IgG preparations from healthy donors are used to treat chronic inflammatory and autoimmune diseases, providing evidence that serum IgG antibodies can have an active immunomodulatory activity. Research over the last two decades has established that the single sugar moiety attached to each IgG heavy chain plays a very important role in modulating the pro- and anti-inflammatory activities of IgG. Moreover, specific sugar moieties such as sialic acid and galactose residues can serve as highly specific biomarkers for ongoing inflammatory processes. This chapter will summarize how different sugar residues in the IgG sugar moiety change upon inflammation and how such changes may translate to altered IgG function and hence maybe useful for optimizing or modulating the function of therapeutic antibodies.© 2025. The Author(s), under exclusive license to Springer Nature Switzerland AG.
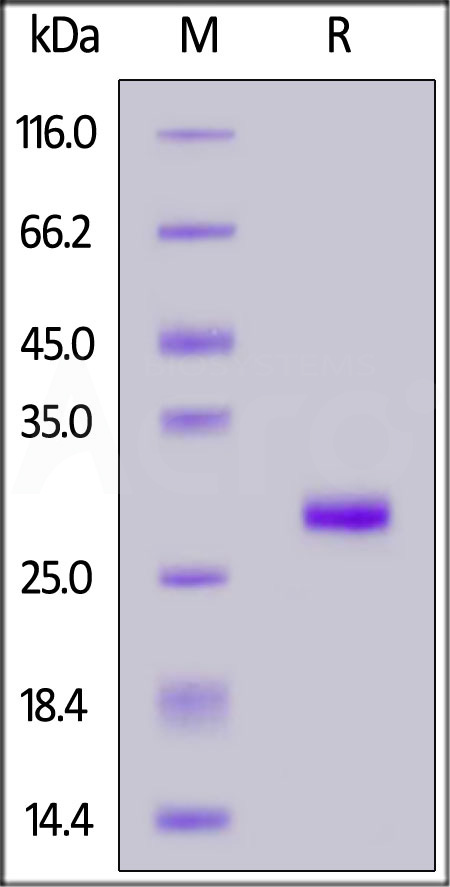
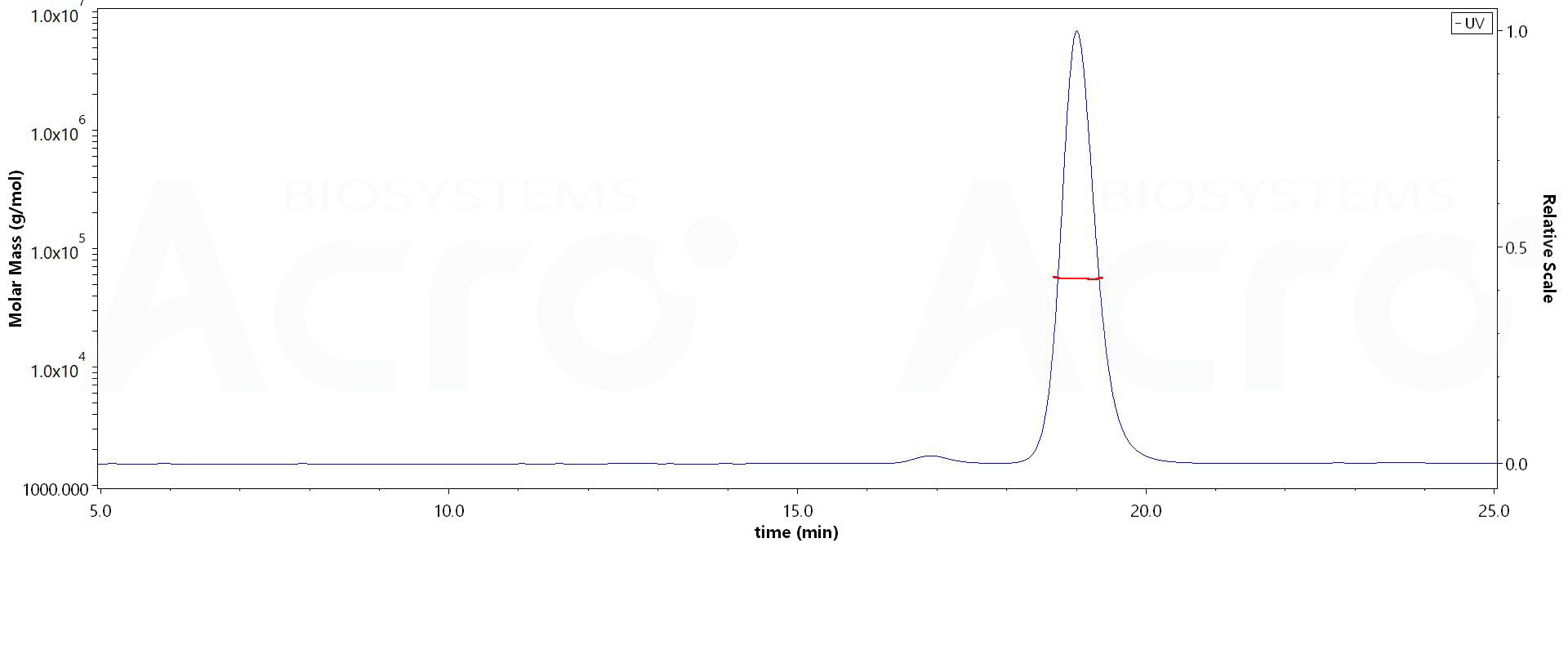
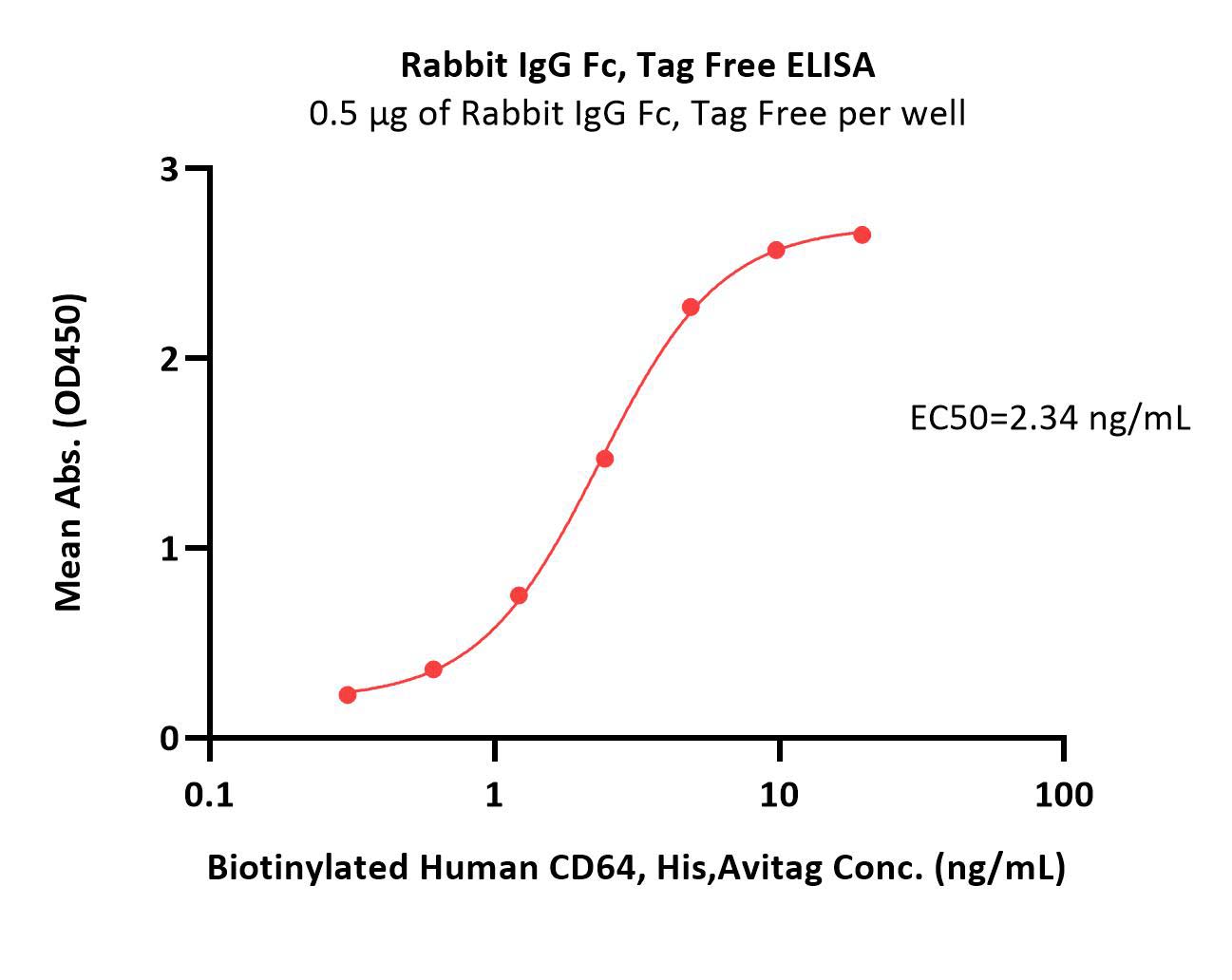























































 膜杰作
膜杰作 Star Staining
Star Staining















