Effects of Space Flight on Inflammasome Activation in the Brain of MiceRoy, Hadad, Rodriguez
et alCells (2025) 14 (6)
Abstract: Space flight exposes astronauts to stressors that alter the immune response, rendering them vulnerable to infections and diseases. In this study, we aimed to determine the levels of inflammasome activation in the brains of mice that were housed in the International Space Station (ISS) for 37 days. C57BL/6 mice were launched to the ISS as part of NASA's Rodent Research 1 Mission on SpaceX-4 CRS-4 Dragon cargo spacecraft from 21 September 2014 to 25 October 2014. Dissected mouse brains from that mission were analyzed by immunoblotting of inflammasome signaling proteins and Electrochemiluminescence Immunoassay (ECLIA) for inflammatory cytokine levels. Our data indicate decreased inflammasome activation in the brains of mice that were housed in the ISS for 37 days when compared to the brains of mice that were maintained on the ground, and in mice corresponding to the baseline group that were sacrificed at the time of launching of SpaceX-4. Moreover, we did not detect any significant changes in the expression levels of the pro-inflammatory cytokines TNF-α, IL-2, IFN-γ, IL-5, IL-6, IL-12p70 and IL-10 between the ground control and the flight groups. Together, these studies suggest that spaceflight results in a decrease in the levels of innate immune signaling molecules that govern inflammasome signaling in the brain of mice.
Effect and Mechanism of Vitamin D on Inflammatory Factors and Neutrophil Activity in Preterm Placenta of Rats Induced by LPSYang, Chen, Lv
Cell Biochem Biophys (2025)
Abstract: To investigate the impact mechanisms of vitamin D on inflammatory factors and neutrophil activity in preterm pregnant rats. 24 pregnant rats were selected as the research objects and randomly divided into control group, LPS group and LPS + VD group, with 8 rats in each group. On the second day of pregnancy, the LPS + VD group was injected intraperitoneally with 50 mg/L vitamin D30.2 mL, and the LPS group and the control group were injected with the same amount of 0.9% NaCl twice a day. On the seventh day of pregnancy, the LPS group and the LPS + VD group were injected with 0.2 mL LPS into the tail vein to establish a preterm labor model induced by infection. The control group was injected with the same amount of physiological saline into the tail vein. Placental tissues from rats in the LPS + VD group and the LPS group were collected, and the expression levels of inflammatory factors TGF-β1, TNF-α, and VDBP were detected by immunohistochemistry. At the same time, serum IL-2 concentration was measured by ELISA and radioimmunoassay, the activity of neutrophils was evaluated by flow cytometry, and the expression of Hippo-YAP signaling pathway protein was detected by Western blot. Compared with the control group, the content of TNF-α, VDBP, and TGF-β1 in placenta in LPS group were higher than that in the control group (P < 5); Compared with the LPS group, the contents of TNF-α, BP and TGF-β1 in the LPS+VD group were significantly reduced,(P < 0.05); Compared with the control group, the serum IL-2 concentration in the LPS group was significantly higher than that in the control group (P < 0.05); Compared with the LPS group, the serum IL-2 concentration in the LPS + VD group decreased significantly (P < 0.05); Compared with the control group, the neutrophil ratio and absolute neutrophil value in the LPS group were higher than those in the control group (P < 0.05); Compared with the LPS group, the neutrophil ratio and absolute value of neutrophils decreased (P < 0.05); compared with the control group, the expression levels of YAP and P-YAP protein in the LPS group increased (P < 0.05); compared with the LPS group, the expression levels of YAP and P-YAP protein in the LPS + VD group decreased (P < 0.05). Vitamin D can improve the immune status of preterm pregnant mice by inhibiting the expression of placental inflammatory factors.© 2025. The Author(s), under exclusive licence to Springer Science+Business Media, LLC, part of Springer Nature.
Serum Interleukin Levels Predict Occurrence of Acute Radiation Pneumonitis and Overall Survival in Thoracic TumoursZhang, Shen, Li
et alClin Invest Med (2025) 48 (1), 29-38
Abstract: Radiation-induced lung injury (RILI) is a significant adverse effect of thoracic radiotherapy, potentially impacting patient prognosis. The risk factors for acute radiation pneumonitis (RP) have not been fully clarified. The present study evaluated the predictive value of serum interleukins (ILs) in the occurrence of RP and overall survival in patients with thoracic cancers.This single-centre retrospective observational study enrolled 435 thoracic cancer patients who underwent chest radiation therapy. Serum levels of IL-1β, IL-2, IL-4, IL-5, IL-6, IL-8, IL-10, IL-12p70, IL-17, TNF-α, IFN-γ, IFN-α were measured by cytometric bead array before radiotherapy. The relationship between clinical characteristics, serum IL levels and the occurrence of RP were analyzed. Cox regression and Kaplan-Meier methods were also performed to investigate the prognostic role of serum IL levels in these patients.The incidence of RP in these patients was 17.01%. Elevated serum levels of IL-1β, IL-2, IL-4, IL-6, IL-8, IL-10, IL-12p70, TNF-α, IFN-α were all associated with the occurrence of RP. High levels of IL-1β, IL-4, and IL-12p70 were correlated with more severe pneumonitis. Univariate and multivariate logistic regression analysis identified serum IL-6 level as an independent prognostic factor in patients receiving thoracic radiotherapy.Serum interleukin levels are linked to the development of acute RP in patients receiving thoracic radiotherapy. Serum IL-6 could serve as a valuable biomarker in identifying patients at high risk for RP, potentially guiding individualized therapeutic strategies and improving patient management in radiotherapy. Future research should focus on validating IL-6's role in larger cohorts and exploring its integration into clinical practice for the early prediction of RILI.
Upregulated TCF1+ Treg Cells With Stronger Function in Systemic Lupus Erythematosus Through Activation of the Wnt-β-CateninZeng, Gao, Bahabayi
et alImmunology (2025)
Abstract: The role of T-cell factor 1 (TCF1) in human regulatory T cells (Treg) and its clinical significance in systemic lupus erythematosus (SLE) remain unclear. Through bioinformatics analysis and flow cytometry, the Tcf7 gene and TCF1 protein were found to be highly expressed in Treg cells. TCF1+ Treg cells exhibited increased expression of CTLA4 and LAG3 and higher IL-10 secretion than TCF1- Treg cells. Circulating TCF1+ Treg cells were elevated and displayed increased inhibitory markers in SLE patients. The Wnt-β-catenin pathway was activated in TCF1+ Treg cells in SLE patients. The addition of XAV939 impaired the function of TCF1+ Treg cells. Clinically, TCF1+ Treg cells were not only related to CRP, ESR and IL-2, but also could differentiate SLE patients from healthy controls, primary Sjögren's syndrome patients and rheumatoid arthritis patients. In conclusion, the increased TCF1+ Treg cells in SLE patients indicate a stronger suppressive function for the activated Wnt-β-catenin pathway and help screening and assisting in the diagnosis of SLE patients.© 2025 John Wiley & Sons Ltd.



 +添加评论
+添加评论















































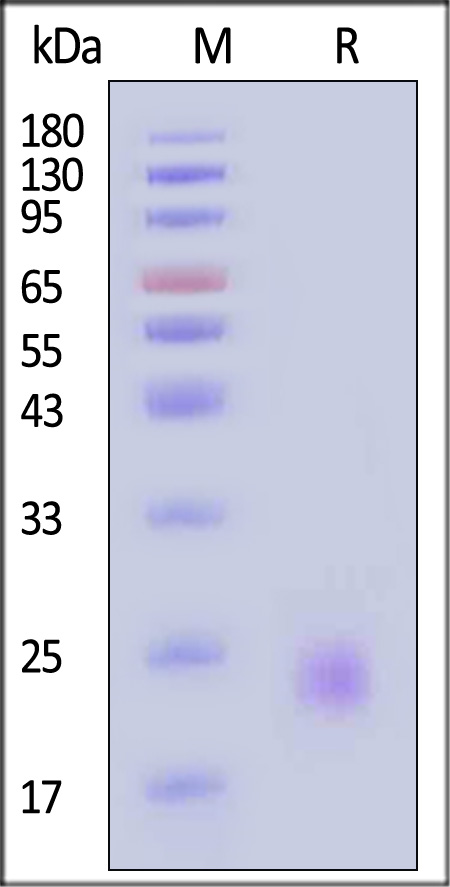
 膜杰作
膜杰作 Star Staining
Star Staining