In-house assays for detecting anti-SARS-CoV-2 antibodies in serum and urine: Correlation with COVID-19 severity from a cohort study in QatarVaikath, Al-Nesf, Majbour
et alJ Infect Public Health (2025) 18 (6), 102744
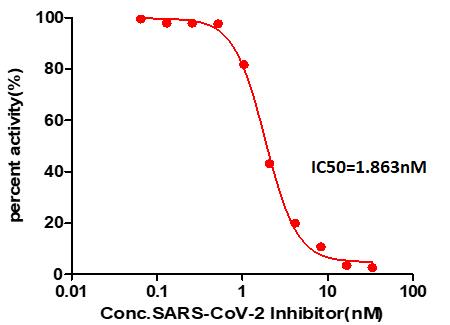
Abstract: Serological assays targeting antibodies against key viral proteins, including the Spike (S1), Receptor Binding Domain (RBD), and Nucleocapsid, play a critical role in understanding immunity and supporting diagnostic efforts during COVID-19 pandemic, and afterward. This study aimed to develop and validate in-house assays for detecting anti-SARS-CoV-2 antibodies in serum and urine.ELISA-based assay was developed to detect IgG and IgM antibodies against SARS-CoV-2. The assay was examined in serum and urine samples of two different cohort of patients affected by COVID-19 disease with different severity and compared to age and sex matched control group. Neutralizing antibody activity was evaluated using an RBD-ACE2 binding inhibition assay. Additionally, a Sengenics protein microarray platform was employed to assess epitope-specific antibody responses.The in-house ELISA assay reliably detected antibodies in both 163 serum and 64 urine samples compared to 50 serum samples from healthy control, with strong correlations observed between antibody levels in the two biofluids. Neutralizing antibody levels correlated positively with disease severity, highlighting their clinical relevance. The performance of the in-house assays was comparable to commercial kits, and the Sengenics microarray provided detailed insights into antibody profiles, identifying dominant epitopes within the Nucleocapsid core domain and RBD.The developed in-house assay demonstrated robust performance and versatility, offering a cost-effective and scalable alternative to commercial kits. Their ability to detect antibodies in both serum and urine highlighted their potential as non-invasive diagnostic tools. These findings contribute to advancing sero-diagnostic capabilities, improving understanding of immune responses to SARS-CoV-2, and supporting global efforts to monitor and manage COVID-19 effectively.Copyright © 2025. Published by Elsevier Ltd.
Impact of pre-existing immunity on humoral and cellular responses to CoronaVac in SARS-CoV-2 variants: A focus on common human CoronavirusesPinpathomrat, Seeyankem, Sophonmanee
et alAsian Pac J Allergy Immunol (2025)
Abstract: The global COVID-19 pandemic, caused by SARS-CoV-2, has highlighted the importance of understanding immune responses elicited by vaccines.This study evaluated antibody and T cell responses to the inactivated CoronaVac vaccine, as well as the role of pre-existing immunity to common human coronaviruses (HCoVs) in shaping vaccine-induced immunity.We enrolled 64 participants (17 males and 47 females) and measured IgG levels against HCoVs before and after vaccination. T cell responses were analysed by stimulating peripheral blood mononuclear cells (PBMCs) with wild-type, Delta, and Omicron spike peptides.We found pre-existing antibodies against HCoV-229E, HCoV-HKU1, HCoV-NL63, and HCoV-OC43 were present before vaccination. Notably, a positive correlation was observed between pre-existing antibodies to HCoV-229E and HCoV-HKU1 and anti-RBD IgG levels post-vaccination. Pre-existing CD4+ T cell responses were observed for the wild-type strain before vaccination, with a significant reduction in IFN-γ secretion after Delta re-stimulation and partial restoration after Omicron re-stimulation. IL-4 production by CD4+ T cells was significantly reduced upon re-stimulation with Delta and Omicron compared to wild-type. CD8+ T cells again showed a reduction of IL-4 production after Delta re-stimulation compared to the original strain.This work demonstrate that CoronaVac induces robust humoral and cellular immune responses, though variant-specific responses vary. Pre-existing immunity to certain HCoVs may influence vaccine-induced antibody responses, underscoring the importance of monitoring immunity to emerging SARS-CoV-2 variants and informing future vaccine design.
Enhanced T-cell immunity and lower humoral responses following 5-dose SARS-CoV-2 vaccination in patients with inborn errors of immunity compared with healthy controlsLopes da Silva, Schmitz, Sullivan
et alFront Immunol (2025) 16, 1538453
Abstract: Patients with Inborn Errors of Immunity (IEI) are at higher risk of severe SARS-CoV-2 infection. We evaluated humoral and cellular responses to COVID-19 vaccines in Brazilian patients with IEI and healthy controls.Fifty-five patients with IEI (13-61 years) and 60 controls (13-71 years) received inactivated SARS-CoV-2 (CoronaVac), non-replicating virus-vectored (ChAdOx1 nCoV-19, AstraZeneca) or monovalent mRNA (Original strain of BNT162b2, Pfizer-BioNTech) and bivalent mRNA (Original/Omicron BA.1, Pfizer-BioNTech) vaccines and were sampled five times. Diagnoses included common variable immunodeficiency (n=25), specific antibody deficiency (n=9), ataxia-telangiectasia (n=5), X-linked agammaglobulinemia (n=4), PIK3CD-related disorders (n=4), hyper-IgM syndrome (n=4), combined immunodeficiency (n=3), and STAT1 gain-of-function (n=1). Humoral immunity was assessed via multiplex microarray for Spike, Nucleocapsid, RBD-Wuhan, RBD-Delta, RBD-BA.1, RBD-BA.2 and RBD-BA.5 neutralizing antibodies. T-cell responses to Spike and Nucleocapsid were assessed using ELISpot.Patients with IEI exhibited significantly lower levels of Nucleocapsid and RBD-neutralizing antibodies (p < 0.05). Notable differences in RBD-BA.2 (p = 0.008) and IgG-Nucleocapsid (p = 0.010) levels emerged over time. T-cell responses to Spike were stronger in patients with IEI post-booster (405 vs. 149 spot-forming cells/million PBMC; p = 0.002). Both groups showed enhanced Nucleocapsid-specific cellular responses over time (p = 0.017). COVID-19 hospitalization rates among patients with IEI with SARS-CoV-2 diagnosis dropped from 33.3% to zero after the first booster dose.While humoral responses to SARS-CoV-2 vaccines were weaker in patients with IEI, their cellular immunity was similar to controls. Boosters enhanced both humoral and cellular responses. After completion of the vaccination protocol, none of the patients with IEI were hospitalized with COVID-19. Robust T-cell responses may play a critical role in protecting patients with IEI from severe COVID-19 and mortality.Copyright © 2025 Lopes da Silva, Schmitz, Sullivan, Barbate, de Haro Azinar, Aranda and de Moraes-Pinto.
Effect of pre-vaccination blood and T-cell phenotypes on antibody responses to COVID-19 mRNA vaccineHidaka, Jo, Kikuchi
et alInt Immunol (2025)
Abstract: Despite the high effectiveness of the coronavirus disease (COVID-19) mRNA vaccines, both immunogenicity and reactogenicity show substantial interindividual variability. One key challenge is predicting high and low responders using easily measurable parameters. In this study, we performed multivariate linear regression analysis, which allows adjustment for confounding, to explore independent predictive factors for antibody responses. Using data from 216 healthy vaccinated donors aged 23-81 years, we evaluated baseline characteristics, pre-vaccination blood and T-cell phenotypes, and post-vaccination T-cell responses as variables, with anti-receptor-binding domain (RBD) immunoglobulin G (IgG) titers following two doses of BNT162b2 vaccination as the primary outcome. Consistent with previous reports, higher age, a history of allergic disease, and autoimmune disease were associated with lower peak IgG titers. Additionally, the frequencies of interferon-γ+ spike-specific CD4+ T cells (T-cell response) following the first vaccination strongly correlated with higher IgG responses, while those of pre-existing spike-reactive T cells showed no association with peak IgG titers. Furthermore, we identified lower percentages of naïve CD8+ T cells, lower hemoglobin levels, lower lymphocyte counts, and higher mean corpuscular volume as independent pre-vaccination predictors of lower peak IgG levels. Notably, the frequency of naïve CD8+ T cells showed a positive correlation with the peak IgG levels even in univariate analysis. These findings contribute to the individualized prediction of mRNA vaccine efficacy and may provide insights into the mechanisms underlying individual heterogeneity in immune responses.© The Author(s) 2025. Published by Oxford University Press on behalf of The Japanese Society for Immunology.























































 膜杰作
膜杰作 Star Staining
Star Staining















