Insights on the Role of Sialic Acids in Acute Lymphoblastic Leukemia in ChildrenRadu, Baek
Int J Mol Sci (2025) 26 (5)
Abstract: Sialic acids serve as crucial terminal sugars on glycoproteins or glycolipids present on cell surfaces. These sugars are involved in diverse physiological and pathological processes through their interactions with carbohydrate-binding proteins, facilitating cell-cell communication and influencing the outcomes of bacterial and viral infections. The role of hypersialylation in tumor growth and metastasis has been widely studied. Recent research has highlighted the significance of aberrant sialylation in enabling tumor cells to escape immune surveillance and sustain their malignant behavior. Acute lymphoblastic leukemia (ALL) is a heterogenous hematological malignancy that primarily affects children and is the second leading cause of mortality among individuals aged 1 to 14. ALL is characterized by the uncontrolled proliferation of immature lymphoid cells in the bone marrow, peripheral blood, and various organs. Sialic acid-binding immunoglobulin-like lectins (Siglecs) are cell surface proteins that can bind to sialic acids. Activation of Siglecs triggers downstream reactions, including induction of cell apoptosis. Siglec-7 and Siglec-9 have been reported to promote cancer progression by driving macrophage polarization, and their expressions on natural killer cells can inhibit tumor cell death. This comprehensive review aims to explore the sialylation mechanisms and their effects on ALL in children. Understanding the complex interplay between sialylation and ALL holds great potential for developing novel diagnostic tools and therapeutic interventions in managing this pediatric malignancy.
Soluble immune checkpoints are dysregulated in patients with sickle cell disease and correlate with inflammatory mediators, autoantibodies, immune cell profiles, and clinical outcomesLi, Pucka, Houran
et almedRxiv (2025)
Abstract: Sickle cell disease (SCD) is a chronic condition characterized by inflammation, immune dysregulation, and debilitating pain.This study investigates soluble immune checkpoints (sICPs) and their associations with inflammatory mediators, immune cell profiles, autoantibodies, and clinical outcomes in SCD.Peripheral blood samples from 50 SCD patients and 40 demographic-matched healthy controls (HCs) were analyzed for 37 sICPs, 80 inflammatory mediators, and 18 autoantibodies using multiplex assays, alongside immune cell profiles via flow cytometry. Pain and quality of life (QoL) were assessed through patient-reported outcome measures (PROMs).Twenty-three sICPs, including arginase-1, BTLA, CD27, CD28, CD47, CD80, CD96, CD134, CD137, CD152, GITR, HVEM, IDO, LAG-3, MICA, MICB, Nectin-2, PD-1, Siglec-7, Siglec-9, TIM-3, TIMD-4, and VISTA, were significantly elevated in SCD patients compared to HCs. These sICPs correlated with multiple proinflammatory mediators (e.g., IL-18), autoantibodies (e.g., MPO), and immune cell activation markers (e.g., CD38/HLA-DR on CD8 T cells). Notably, CD28, CD152, HVEM, and VISTA were strongly associated with systemic inflammation and immune cell activation, while BTLA, LAG-3, PD-1, and CD80 correlated with pain and anxiety scores and QoL.This study highlights complex interactions between sICPs, immune activation, inflammation, and clinical outcomes in SCD, underscoring their potential as biomarkers or therapeutic targets to alleviate inflammation and improve QoL in this challenging clinical population.
HIV-Induced Sialoglycans on Infected Cells Promote Immune Evasion from Myeloid Cell-Mediated KillingSingh, Islam, Liu
et albioRxiv (2025)
Abstract: Sialic acid-containing glycans (sialoglycans) on pathological cells interact with Siglecs, glycol-immune checkpoint receptors expressed on myeloid cells such as monocytes and neutrophils. This interaction suppresses the cytotoxic functions of these immune cells. We show that HIV infection reprograms the glycosylation machinery of infected cells to increase the expression of specific sialoglycan ligands for Siglecs-3, -7, and -9. These ligands engage Siglecs on myeloid cells, impairing their ability to target HIV-infected cells. Selective disruption of these interactions using 10-1074-Sia, an HIV-specific antibody conjugated to sialidase-an enzyme that removes sialic acids-significantly enhances monocyte- and neutrophil-mediated killing of HIV-infected cells in autologous assays. Treatment with 10-1074-Sia in humanized mice infected with HIV reduces viral load and decreases inflammation. These findings reveal a novel immune evasion mechanism exploited by HIV to evade myeloid cell immune surveillance and highlight the potential of targeting sialoglycan-Siglec interactions to improve immune clearance of HIV-infected cells.
[Preliminary study on the role of siglec-9 expression in peripheral blood of acute respiratory distress syndrome patients]Liu, Lu, Cai
et alZhonghua Jie He He Hu Xi Za Zhi (2025) 48 (2), 123-129
Abstract: Objective: Sialic acid-binding immunoglobulin-like lectin (siglec)-9 is a type Ⅰ transmembrane protein that plays an important role in intrinsic immunity. In this study, we examined the siglec-9 expression levels in mononuclear macrophages, neutrophils and plasma from peripheral blood of acute respiratory distress syndrome (ARDS) patients and investigated its clinical value. Methods: Peripheral blood was obtained from ARDS patients (n=54) admitted to the Department of Respiratory and Critical Care Medicine, Nanjing Jinling Hospital and the Second People's Hospital of Wuhu, Anhui Province, China, from July 2021 to October 2022. Healthy volunteers (n=50) from the physical examination center and hospitalized patients (n=47) with lung infection were included as control groups. The expression of cellular and plasma siglec-9 was detected by flow cytometry and ELISA separately. Results: Compared with lung infection group and healthy control group, the expression of monocytes and plasma siglec-9 in ARDS group increased significantly. But there was no significant difference in the expression of monocytes and plasma siglec-9 between lung infection group and healthy control group. The level of plasma siglec-9 was significantly higher in moderate-severe ARDS patients than that in mild patients (P<0.05). Multivariable logistic regression analysis showed that IL-6, LDH and plasma siglec-9 were independent risk factors of ARDS, while plasma siglec-9, IL-6 and APACHE Ⅱ were independent risk factors of moderate-severe ARDS. Conclusion: The expression of siglec-9 in the plasma of ARDS patients is positively correlated with the severity of ARDS, which has a certain value in the assessment of ARDS.

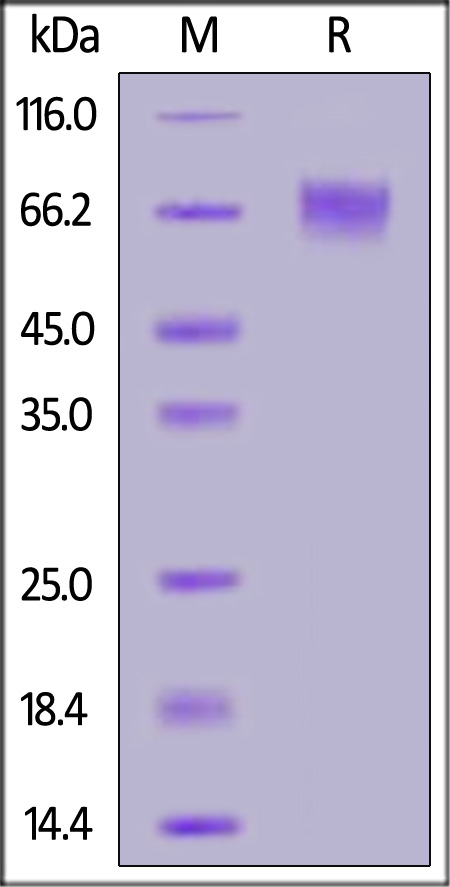























































 膜杰作
膜杰作 Star Staining
Star Staining