Astragaloside IV Relieves Mitochondrial Oxidative Stress Damage and Dysfunction in Diabetic Mice Endothelial Progenitor Cells by Regulating the GSK-3β/Nrf2 AxisZou, Liu, Qu
et alAppl Biochem Biotechnol (2025)
Abstract: Dysregulation of mitochondrial activity is a major cause of diabetes mellitus (DM) and its complications. Astragaloside IV, a natural herbal product, possesses protective properties against DM. This study aimed to evaluate how astragaloside IV affects oxidative stress and mitochondrial function in endothelial progenitor cells (EPCs) and elucidate the underlying mechanisms. A high glucose (HG)-induced human EPC (hEPC) model and a streptozotocin (STZ)-induced DM mouse model were established to investigate the effects of astragaloside IV on EPC function and wound healing in the context of DM. In HG-exposed hEPCs, astragaloside IV reduced apoptosis and increased cell viability and tube formation (P < 0.05). In STZ-induced DM mice, astragaloside IV promoted wound healing and increased the expression of the endothelial marker CD31 (P < 0.05) in wound tissues. In addition, the regulation of oxidative damage and mitochondrial dysfunction by astragaloside IV was investigated. We found that astragaloside IV attenuated mitochondrial damage, decreased ROS and mtROS levels (P < 0.05), decreased MDA activity and enhanced SOD activity (P < 0.05), and downregulated DPR1 levels and upregulated MFN1, MFN2, and OPA1 levels (P < 0.05). Mechanistically, the potential involvement of GSK-3β/Nrf2 was investigated by molecular docking and intervention with the GSK-3β activator sodium nitroprusside (SNP). Astragaloside IV was confirmed to dock with GSK-3β, and it increased the phosphorylation of GSK-3β (P < 0.05) and the expression of Nrf2 as well as its downstream factors HO-1 and NQO1 (P < 0.05). SNP reversed the protective effects of astragaloside IV. These results indicated that astragaloside IV attenuated HG- and STZ-induced injury through the GSK-3β/Nrf2 pathway. These results revealed that astragaloside IV may have the potential to be an active component for protection against DM and its complications.© 2025. The Author(s), under exclusive licence to Springer Science+Business Media, LLC, part of Springer Nature.
Microstructural Effects of Melt Electrowritten-Reinforced Hydrogel Scaffolds for Engineering Thick Skin SubstitutesAfghah, Altunbek, Zahrabi
et alACS Appl Bio Mater (2025)
Abstract: Engineering thick skin tissue substitutes resembling the physiochemical and mechanical properties of native tissue is a significant challenge. Melt electrowriting (MEW) is a powerful technique with the capability of fabricating highly ordered structures with fine fiber diameters, closely replicating the native extracellular matrix (ECM). In this study, we constructed melt electrowritten porous polycaprolactone (PCL) scaffolds with three different geometries by depositing fibers at 0-90 and 60-120° in a mesh structure and in a honeycomb-like orientation to assess the effects of the microstructure on the mechanical strength of the scaffold and cellular behavior. These scaffolds were subsequently infilled with gelatin hydrogel, encapsulating human skin dermal fibroblasts (HSFs) and human umbilical vein endothelial cells (HUVECs). Mechanical tensile tests revealed that the honeycomb microstructure of the hybrid PCL/gelatin scaffold exhibited greater elongation at failure, along with an acceptable elastic modulus suitable for skin tissue applications. All scaffolds provided a cytocompatible microenvironment that maintained over 90% cell viability and preserved typical cell morphology. HSFs were guided through the PCL fibers to the apical surface, while HUVECs were distributed within the gelatin hydrogel within the hybrid structure. Additionally, HSFs' alignment was regulated by the scaffold geometry. Notably, the expression of CD31 in HUVECs─a key transmembrane protein for capillary formation─increased significantly over a 14 day incubation period. Among those, 0-90° mesh and honeycomb geometries showed the greatest effects on the upregulation of CD31. These findings demonstrate that the microstructural guidance of HSFs and their interaction with HUVECs in hybrid structures play a crucial role in promoting vascularization. In conclusion, the honeycomb MEW-gelatin hybrid scaffold demonstrates significant potential for effectively replicating both the mechanical and physicochemical properties essential for full-thickness skin tissue substitutes.
A novel rat model of lumbar disc herniation induced by puncture: accurate positioning and controllable degree of herniationYang, Zhou, Yang
et alJ Orthop Surg Res (2025) 20 (1), 309
Abstract: Lumbar disc herniation (LDH) is the serious stage of intervertebral disc degeneration (IDD), and the location and degree of intervertebral disc herniation are closely related to clinical symptoms and signs. However, there is currently no low-cost, high-benefit animal model to support in vivo research on LDH.Expose the rat's lumbar 5/6 intervertebral disc through the space between the psoas major and erector spine muscles, and then use different lengths of puncture needles to control the degree of herniation and different puncture angles to push the nucleus pulposus tissue backwards to the different position. Observe the protrusion of intervertebral discs through MRI. Von Frey mechanical pain test and BBB score were used to evaluate the behavior of LDH rats. H&E and SF staining were used to observe the morphological changes after intervertebral disc herniation. Immunofluorescence was used to analyze the expression of Aggrecan (ACAN), IL-1β, TNF-α, and CD31 in intervertebral disc tissue.LDH rat exhibit varying degrees of motor and sensory dysfunction. The nucleus pulposus tissue in the center of the intervertebral disc undergoes degenerative changes, with a decrease in the content of nucleus pulposus cells and proteoglycans, an increase in the expression of inflammatory factors in the protruding tissue, and neovascularization.We have successfully constructed rat models of different types of intervertebral disc herniation, including disc degeneration, bulging, central herniation, and lateral herniation, using the method of puncture of intervertebral discs. This animal model is consistent with the characteristics of LDH in terms of behavior, imaging, and histopathology.© 2025. The Author(s).
The Association Between Dysglycemia and Endotheliopathy in ICU Patients With and Without Diabetes: A Cohort StudyGantzel Nielsen, Olsen, Lommer Kristensen
et alCrit Care Explor (2025) 7 (4), e1229
Abstract: Dysglycemia in critically ill patients is associated with endotheliopathy. This relationship may be altered in patients with diabetes.Dysglycemia is common in critically ill patients and associated with increased mortality. Endotheliopathy is thought to play a role in this relationship; however, evidence is scarce. The aim of this study was to investigate the associations between dysglycemia and endotheliopathy to inform future glycemic management.This prospective observational study included 577 acutely admitted adult ICU patients at Copenhagen University Hospital-North Zealand, Denmark.Up to twenty-four hours of patient glycemia was paired with same-day levels of endothelial biomarkers measured after each 24-hour period for three consecutive days. Endotheliopathy was assessed by measurement of Syndecan-1, Platelet Endothelial Cell Adhesion Molecule-1 (PECAM-1), and soluble thrombomodulin (sTM).Of the included patients, a total 57.5% were males, median age was 71 yr (interquartile range [IQR], 63-79), and 24.6% had diabetes prior to admission. Median admission time was 5 d (IQR, 3-10). Time above range (TAR) greater than 13.9 mmol/L, but not TAR 10.0-13.9 mmol/L, was associated with increase in sTM (0.01 ng/mL per %-point increase in TAR, p = 0.049) and PECAM-1 (0.01 ng/mL per %-point increase, p = 0.007). Glycemic variability was associated with increases in sTM (0.24 ng/mL per mmol/L increase in sd, p = 0.001 and 0.03 ng/mL per %-point increase in coefficient of variation, p < 0.001). Hypoglycemia 3.0-3.9 mmol/L was associated with increases in sTM (3.0 ng/mL, p < 0.001) and PECAM-1 (1.54 ng/mL, p < 0.001).In acutely admitted adult ICU patients, hypoglycemia was associated with endotheliopathy regardless of preadmission diabetes status. Hyperglycemia and high glycemic variability were associated with endotheliopathy in patients without diabetes. This suggests different responses to acute dysglycemia in patients with and without diabetes and warrants further investigation in clinical trials.Copyright © 2025 The Authors. Published by Wolters Kluwer Health, Inc. on behalf of the Society of Critical Care Medicine.

 +添加评论
+添加评论























































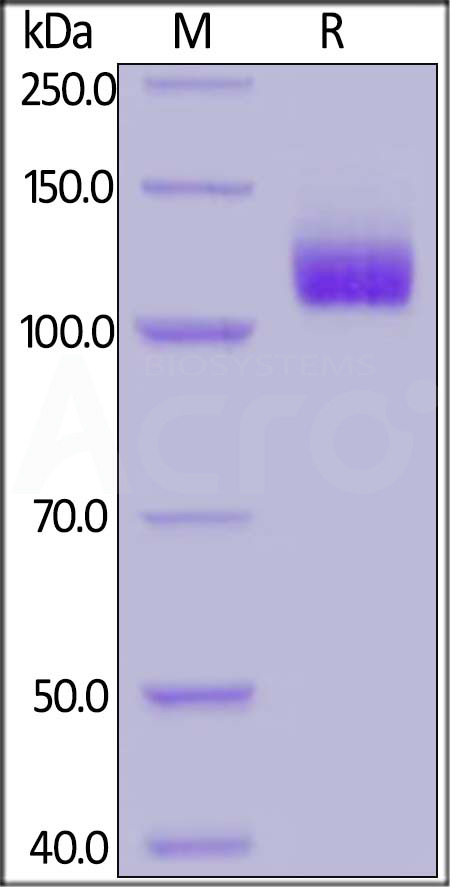
 膜杰作
膜杰作 Star Staining
Star Staining