Inhibition of Activin A suppressed tumor necrosis factor-α secretion and improved histopathological conditions in malarial miceChin, Tie, Abd Majid
et alTrop Biomed (2021) 38 (1), 187-204
Abstract: Malaria infection still remains as one of the most prominent parasitic diseases afflicting mankind in tropical and subtropical regions. The severity of malaria infection has often been associated to exuberant host immune inflammatory responses that could possibly lead to severe immunopathological conditions and subsequent death of host tissues. Activin A is a protein belonging to the transforming growth factor-beta (TGF-β) family that regulates multiple physiological processes and pathological-associated diseases. The biological roles of activin A have been associated with manipulation of inflammation-related processes and modulation of host immune responses. This implies that activin A protein could play a role in malaria pathogenesis since malaria infection has been closely linked to severe immune responses leading to death, However, the actual in vivo role of activin A in malaria infection remains elusive. Hence, this study was undertaken to investigate the involvement of activin A in malaria infection as well as to assess the modulating effects of activin A on the cytokine releases (TNF-α, IFN-γ and IL-10) and histopathological changes in major affected organs (kidney, liver, lung, brain and spleen) in malarial mice infected with Plasmodium berghei ANKA. Our results showed that the concentrations of plasma activin A were significantly increased in malarial mice throughout the study periods. Also. the systemic activin A level was positively correlated with malaria parasitemia. This indicates that activin A could play a role in malaria pathogenesis and malaria parasitemia development. Plasma TNF-α, IFN-γ and IL-10 cytokine levels were significantly increased in malarial mice at day-5 post infection, suggesting that these cytokines attributed to severe malaria pathogenesis. Histopathological features such as sequestration of parasitized red blood cells (pRBCs) and hemozoin formation were amongst the most common pathological conditions observed in tissues of major affected organs (kidney, liver, lung, brain and spleen) in malarial mice. Neutralization of activin A production via recombinant mouse activin RIIA Fc chimera (rmActivin RIIA Fc chimera) had significantly reduced the parasitemia levels in malarial mice. The release of TNF-α cytokine was significantly reduced as well as the sequestration of parasitized pRBCs and hemozoin formation in major affected organs in malarial mice were also alleviated following inhibition of activin A production. Overall, this preliminary study suggests that activin A could play an immune modulation role in malaria pathogenesis through modulation of TNF-α release that benefits host from severe pathological destructions provoked by intensified inflammatory responses. Further studies are warranted to elucidate the precise mechanism of immune modulation mediated by activin A and its associated immune-modulation mediators in regulating the inflammatory responses elicited during the course of malaria infection.
Molecular characterization of inhibin-A: Structure and expression analysis in Clarias batrachusAhmad, Jagtap, Selvaa Kumar
et alGen Comp Endocrinol (2018) 261, 104-114
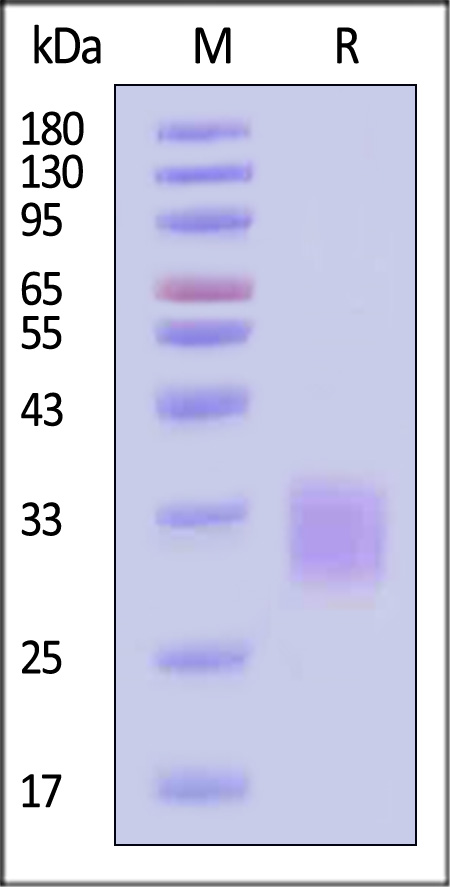
Abstract: The inhibins are disulphide-linked heterodimeric glycoproteins that belong to the TGFβ superfamily. Inhibins have been well studied in mammals but the information about their structure and function is very limited in lower vertebrates. The aim of the present study was to characterize inhibin-A and to understand its receptor binding interaction, and to evaluate its biological function in Clarias batrachus. Structure prediction of inhibin-A revealed two glycosylation sites on inhibin-α (Asp262 and Asn334). Docking of inhibin-A with its receptor; betaglycan and Act RIIA showed that residues Ser321, Gly324 and Leu325 of inhibin-α are involved in high affinity binding with betaglycan while inhibin-βA bound to Act RIIA by forming hydrogen bonds. The mRNA transcript analysis of various tissues indicated the presence of higher to moderate expression of inhibin-α and inhibin-βA in the gonads and the extra-gonadal tissues. Further, stage specific expression showed decreased levels of inhibin-α in the gonads during the annual reproductive cycles. Inhibin-βA, activin-βB and Act RIIA increased in the brain during spawning while FSHr increased in the gonads during the preparatory phase. Our study provides molecular, structural and functional insights of inhibin-A for the first time in C. batrachus.Copyright © 2018 Elsevier Inc. All rights reserved.
A Pdx-1-Regulated Soluble Factor Activates Rat and Human Islet Cell ProliferationHayes, Zhang, Becker
et alMol Cell Biol (2016) 36 (23), 2918-2930
Abstract: The homeodomain transcription factor Pdx-1 has important roles in pancreas and islet development as well as in β-cell function and survival. We previously reported that Pdx-1 overexpression stimulates islet cell proliferation, but the mechanism remains unclear. Here, we demonstrate that overexpression of Pdx-1 triggers proliferation largely by a non-cell-autonomous mechanism mediated by soluble factors. Consistent with this idea, overexpression of Pdx-1 under the control of a β-cell-specific promoter (rat insulin promoter [RIP]) stimulates proliferation of both α and β cells, and overexpression of Pdx-1 in islets separated by a Transwell membrane from islets lacking Pdx-1 overexpression activates proliferation in the untreated islets. Microarray and gene ontology (GO) analysis identified inhibin beta-B (Inhbb), an activin subunit and member of the transforming growth factor β (TGF-β) superfamily, as a Pdx-1-responsive gene. Overexpression of Inhbb or addition of activin B stimulates rat islet cell and β-cell proliferation, and the activin receptors RIIA and RIIB are required for the full proliferative effects of Pdx-1 in rat islets. In human islets, Inhbb overexpression stimulates total islet cell proliferation and potentiates Pdx-1-stimulated proliferation of total islet cells and β cells. In sum, this study identifies a mechanism by which Pdx-1 induces a soluble factor that is sufficient to stimulate both rat and human islet cell proliferation.Copyright © 2016, American Society for Microbiology. All Rights Reserved.
Experimental and investigational therapies for chemotherapy-induced anemiaTesta, Castelli, Elvira
Expert Opin Investig Drugs (2015) 24 (11), 1433-45
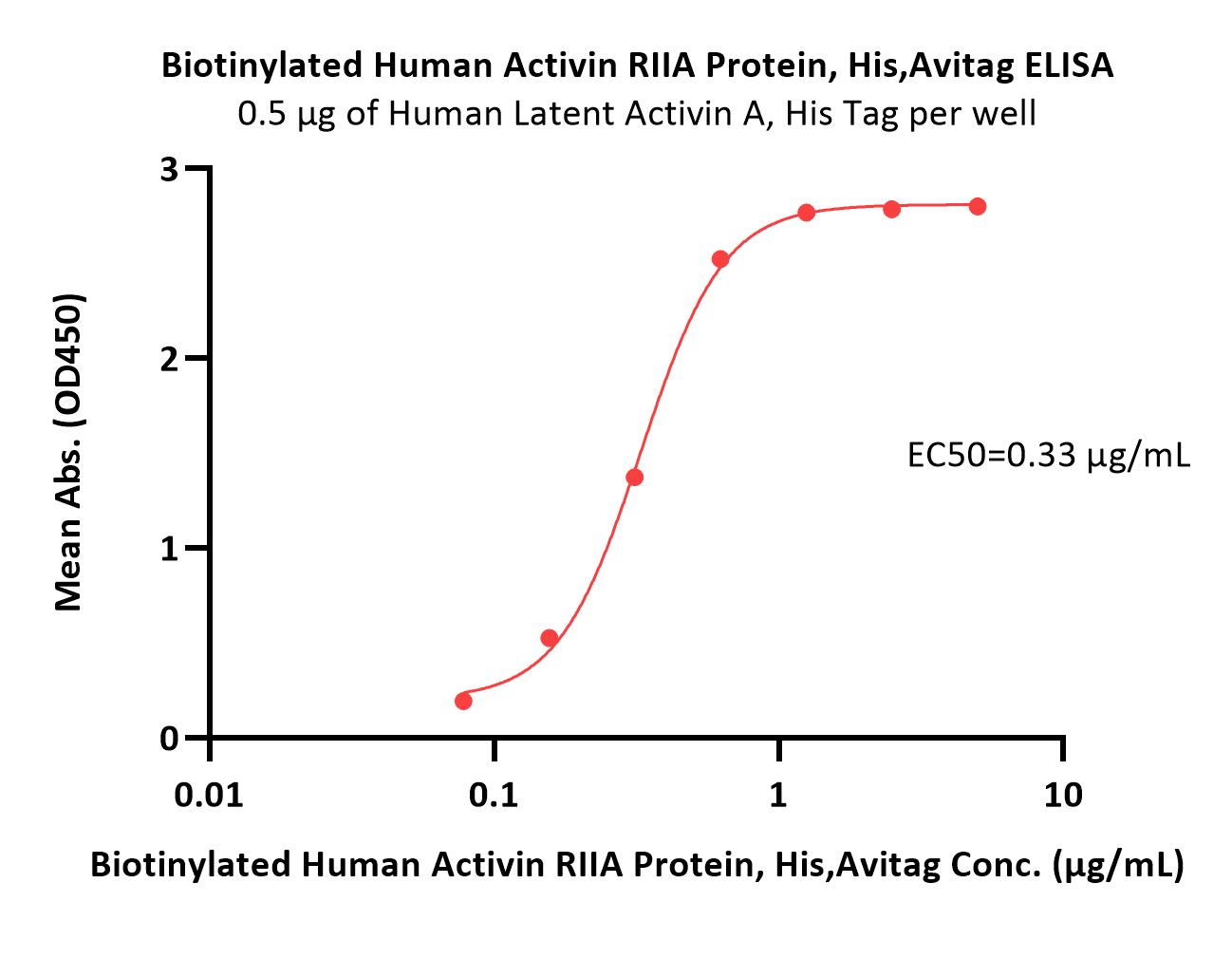
Abstract: In cancer patients, anemia is frequently observed, particularly as a consequence to chemotherapy (chemotherapy-induced anemia, CIA). CIA is treated with Red Blood Cell transfusions and erythropoiesis-stimulating agents (ESAs). However, the use of ESAs in anemic cancer patients is associated with reduced survival time and time to progression. Consequently, new therapeutic options are needed.In this article, the authors discuss new erythroid-enhancing agents (EEAs) that act differently to erythropoietin. Specifically, the article summarizes the early clinical development of activin antagonists (Sotatercep [ACE-011] and ACE-536) and hepcidin antagonists [NOX-H94]).Both Activin RIIA trap agents and hepcidin inhibitors are promising new EEAs, but their safety profile, and their impact on treating CIA, needs to be carefully assessed in controlled clinical trials over longer periods of time. It is also important to carefully evaluate CIA patients to properly assess the physiopathological mechanisms responsible for the development of their anemic condition and provide patients with the most appropriate treatment plan.
 +添加评论
+添加评论






















































 膜杰作
膜杰作 Star Staining
Star Staining














