Preclinical in vitro evaluation of immune suppression induced by GYM329, Fc-engineered sweeping antibodyIwata, Katada, Okuda
et alJ Toxicol Sci (2023) 48 (7), 399-409
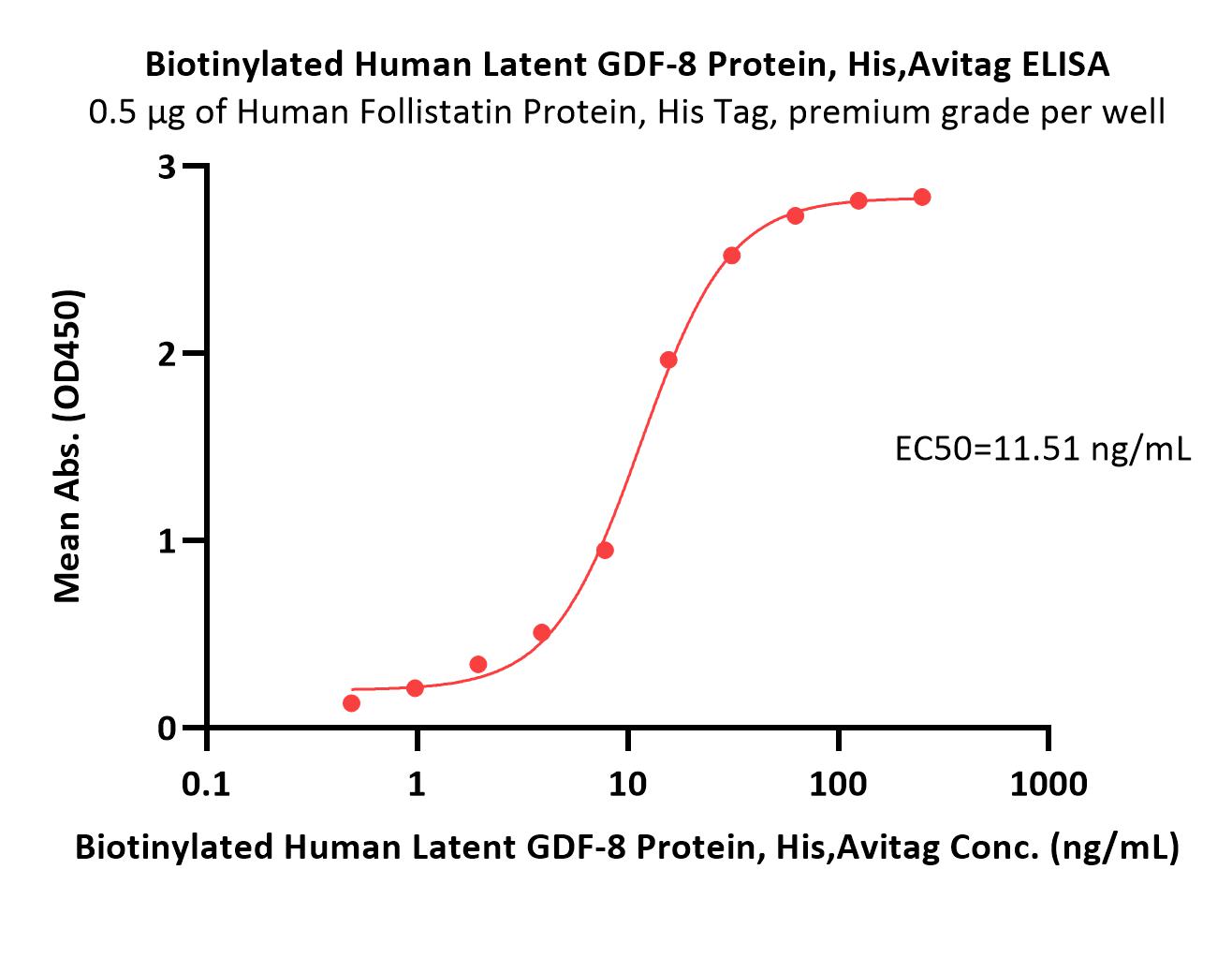
Abstract: Fc-engineering is commonly used to improve the therapeutic potency of antibody (Ab) treatments. Because FcγRIIb is the only inhibitory FcγR that contains an immunoreceptor tyrosine-based inhibition motif (ITIM), Fc-engineered Abs with enhanced binding affinity to FcγRIIb might provide immune suppression in clinical contexts. GYM329 is an anti-latent myostatin Fc-engineered Ab with increased affinity to FcγRIIb which is expected to improve muscle strength in patients with muscular disorders. Cross-linking of FcγRIIb by immune complex (IC) results in phosphorylation of ITIM to inhibit immune activation and apoptosis in B cells. We examined whether the IC of Fc-engineered Abs with enhanced binding affinity to FcγRIIb causes phosphorylation of ITIM or B cell apoptosis using GYM329 and its Fc variant Abs in human and cynomolgus-monkey (cyno) immune cells in vitro. IC of GYM329 with enhanced binding affinity to human FcγRIIb (×5) induced neither ITIM phosphorylation nor B cell apoptosis. As for GYM329, FcγRIIb should work as an endocytic receptor of small IC to sweep latent myostatin, so it is preferable that GYM329 induces neither ITIM phosphorylation nor B cell apoptosis to prevent immune suppression. In contrast, IC of myo-HuCy2b, the Ab with enhanced binding affinity to human FcγRIIb (×4), induced ITIM phosphorylation and B cell apoptosis. The result of the present study demonstrated that Fc-engineered Abs with similar binding affinity to FcγRIIb had different effects. Thus, it is important to also investigate FcγR-mediated immune functions other than binding to fully understand the biological effects of Fc-engineered Abs.
Advances and limitations for the treatment of spinal muscular atrophyDay, Howell, Place
et alBMC Pediatr (2022) 22 (1), 632
Abstract: Spinal muscular atrophy (5q-SMA; SMA), a genetic neuromuscular condition affecting spinal motor neurons, is caused by defects in both copies of the SMN1 gene that produces survival motor neuron (SMN) protein. The highly homologous SMN2 gene primarily expresses a rapidly degraded isoform of SMN protein that causes anterior horn cell degeneration, progressive motor neuron loss, skeletal muscle atrophy and weakness. Severe cases result in limited mobility and ventilatory insufficiency. Untreated SMA is the leading genetic cause of death in young children. Recently, three therapeutics that increase SMN protein levels in patients with SMA have provided incremental improvements in motor function and developmental milestones and prevented the worsening of SMA symptoms. While the therapeutic approaches with Spinraza®, Zolgensma®, and Evrysdi® have a clinically significant impact, they are not curative. For many patients, there remains a significant disease burden. A potential combination therapy under development for SMA targets myostatin, a negative regulator of muscle mass and strength. Myostatin inhibition in animal models increases muscle mass and function. Apitegromab is an investigational, fully human, monoclonal antibody that specifically binds to proforms of myostatin, promyostatin and latent myostatin, thereby inhibiting myostatin activation. A recently completed phase 2 trial demonstrated the potential clinical benefit of apitegromab by improving or stabilizing motor function in patients with Type 2 and Type 3 SMA and providing positive proof-of-concept for myostatin inhibition as a target for managing SMA. The primary goal of this manuscript is to orient physicians to the evolving landscape of SMA treatment.© 2022. The Author(s).
Selective Myostatin Inhibition Spares Sublesional Muscle Mass and Myopenia-Related Dysfunction after Severe Spinal Cord Contusion in MiceBigford, Donovan, Webster
et alJ Neurotrauma (2021) 38 (24), 3440-3455
Abstract: Clinically relevant myopenia accompanies spinal cord injury (SCI), and compromises function, metabolism, body composition, and health. Myostatin, a transforming growth factor (TGF)β family member, is a key negative regulator of skeletal muscle mass. We investigated inhibition of myostatin signaling using systemic delivery of a highly selective monoclonal antibody - muSRK-015P (40 mg/kg) - that blocks release of active growth factor from the latent form of myostatin. Adult female mice (C57BL/6) were subjected to a severe SCI (65 kdyn) at T9 and were then immediately and 1 week later administered test articles: muSRK-015P (40 mg/kg) or control (vehicle or IgG). A sham control group (laminectomy only) was included. At euthanasia, (2 weeks post-SCI) muSRK-015P preserved whole body lean mass and sublesional gastrocnemius and soleus mass. muSRK-015P-treated mice with SCI also had significantly attenuated myofiber atrophy, lipid infiltration, and loss of slow-oxidative phenotype in soleus muscle. These outcomes were accompanied by significantly improved sublesional motor function and muscle force production at 1 and 2 weeks post-SCI. At 2 weeks post-SCI, lean mass was significantly decreased in SCI-IgG mice, but was not different in SCI-muSRK-015P mice than in sham controls. Total energy expenditure (kCal/day) at 2 weeks post-SCI was lower in SCI-immunoglobulin (Ig)G mice, but not different in SCI-muSRK-015P mice than in sham controls. We conclude that in a randomized, blinded, and controlled study in mice, myostatin inhibition using muSRK-015P had broad effects on physical, metabolic, and functional outcomes when compared with IgG control treated SCI animals. These findings may identify a useful, targeted therapeutic strategy for treating post-SCI myopenia and related sequelae in humans.
Preclinical Safety Assessment and Toxicokinetics of Apitegromab, an Antibody Targeting Proforms of Myostatin for the Treatment of Muscle-Atrophying DiseaseWelsh, Cote, Meshulam
et alInt J Toxicol (2021) 40 (4), 322-336
Abstract: Myostatin is a negative regulator of skeletal muscle and has become a therapeutic target for muscle atrophying disorders. Although previous inhibitors of myostatin offered promising preclinical data, these therapies demonstrated a lack of specificity toward myostatin signaling and have shown limited success in the clinic. Apitegromab is a fully human, monoclonal antibody that binds to human promyostatin and latent myostatin with a high degree of specificity, without binding mature myostatin and other closely related growth factors. To support the clinical development of apitegromab, we present data from a comprehensive preclinical assessment of its pharmacology, pharmacokinetics, and safety across multiple species. In vitro studies confirmed the ability of apitegromab to inhibit the activation of promyostatin. Toxicology studies in monkeys for 4 weeks and in adult rats for up to 26 weeks showed that weekly intravenous administration of apitegromab achieved sustained serum exposure and target engagement and was well-tolerated, with no treatment-related adverse findings at the highest doses tested of up to 100 mg/kg and 300 mg/kg in monkeys and rats, respectively. Additionally, results from an 8-week juvenile rat study showed no adverse effects on any endpoint, including neurodevelopmental, motor, and reproductive outcomes at 300 mg/kg administered weekly IV. In summary, the nonclinical pharmacology, pharmacokinetic, and toxicology data demonstrate that apitegromab is a selective inhibitor of proforms of myostatin that does not exhibit toxicities observed with other myostatin pathway inhibitors. These data support the conduct of ongoing clinical studies of apitegromab in adult and pediatric patients with spinal muscular atrophy (SMA).
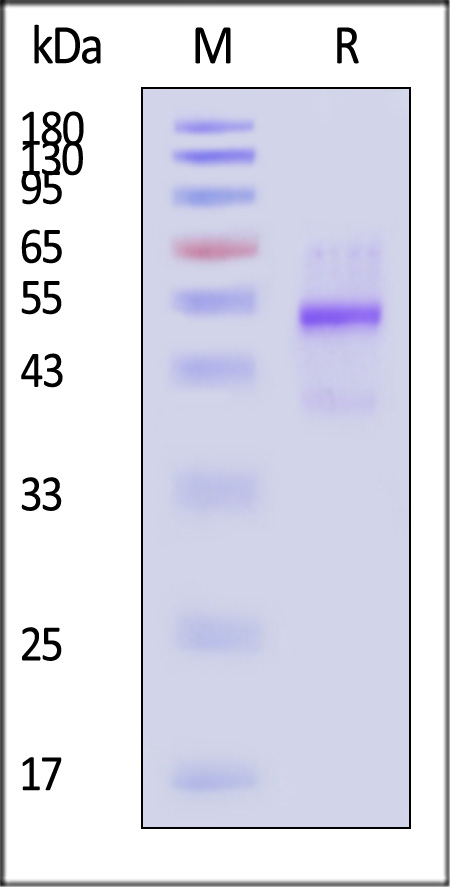
























































 膜杰作
膜杰作 Star Staining
Star Staining















