Progenitor cells and circulating endothelial cells are associated with disease activity and damage in systemic lupus erythematosus patientsSilveira, Ranero, Carlomagno
et alLupus (2025)
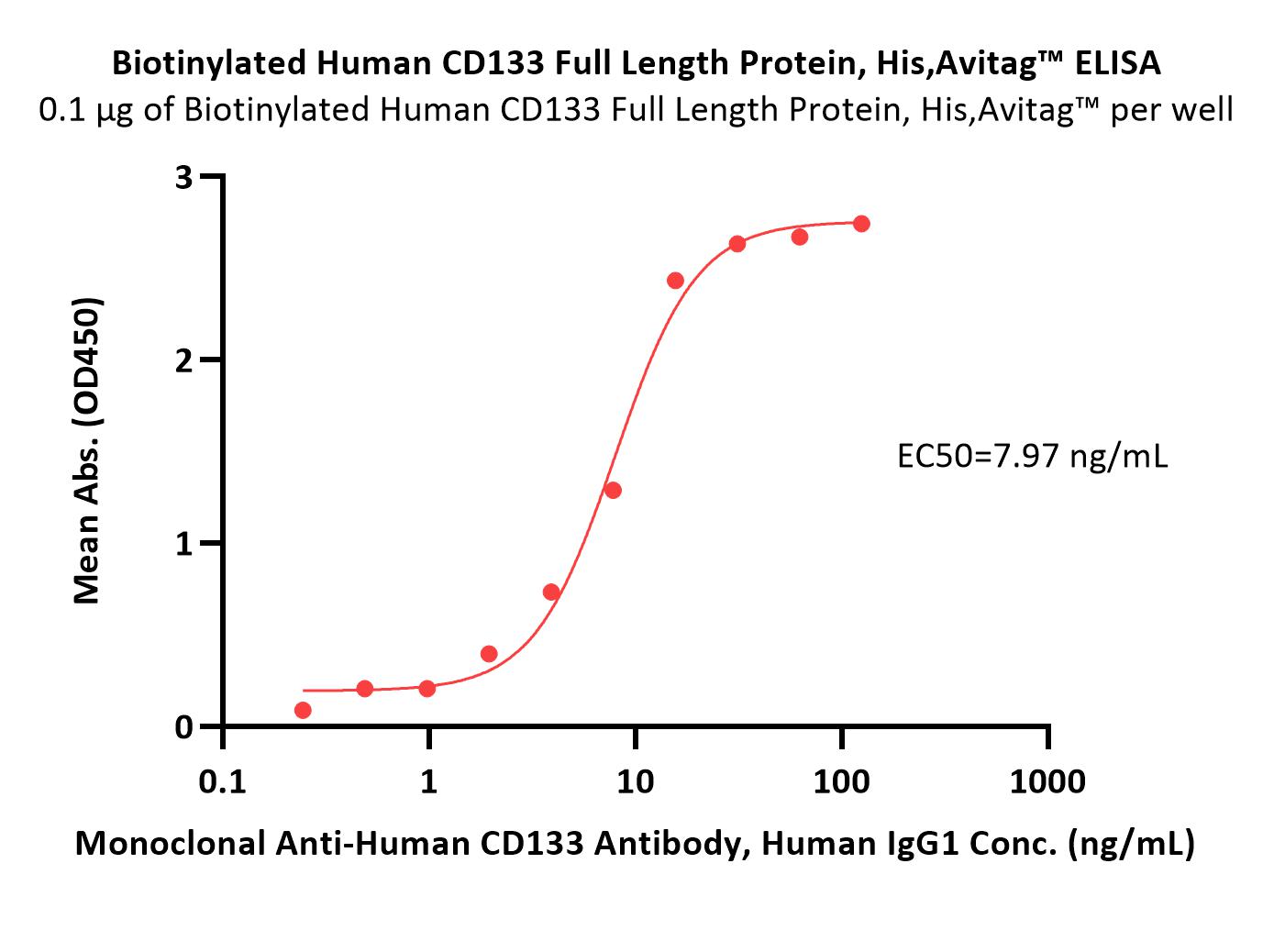
Abstract: BackgroundDespite advancements in treatment, patients with Systemic Lupus Erythematosus (SLE) frequently experience disease flares, which contribute to organ damage and increase the risk of premature death. Assessing disease activity is essential for optimizing treatment and preventing further organ damage. This study aimed to investigate the relationship between levels of progenitor and circulating endothelial cells and SLE disease activity, as well as accumulated organ damage.MethodsWe conducted a case-control study measuring levels of CD34+CD45low/- progenitor cells, CD34+CD45low/-CD133+ progenitor cells, Endothelial Progenitor Cells (EPC), and Circulating Endothelial Cells (CEC) in peripheral blood using flow cytometry.ResultsThe study included 32 SLE patients and 28 matched controls. SLE patients exhibited significantly lower levels of CD34+CD45low/- progenitor cells (p = .001), CD34+CD45low/-CD133+ progenitor cells (p = .016), EPC (p = .018), and CEC (p < .001) compared to controls. Additionally, the cell subpopulations correlated with SLE activity biomarkers, with CD34+CD45low/- progenitor cells showing a moderate negative correlation with C3 and C4 levels. Notably, patients with an SDI score ≥1 had significantly higher levels of CD34+CD45low/- progenitor cells, CD34+CD45low/- CD133+ progenitor cells, EPC, and CEC compared to those without organ damage (p = .0073, p = .018, p = .018, and p = .020, respectively).ConclusionOur findings reveal that CD34+CD45low/- progenitor cells, CD34+CD45low/-CD133+ progenitor cells, EPC, and CEC are significantly reduced in SLE patients and are associated with disease activity and organ damage. These results suggest that CD34+CD45low/- progenitor cells, in particular, could serve as potential biomarkers for monitoring disease activity and organ damage in SLE patients. Prospective studies are warranted to confirm these findings.
Role of octamer transcription factor 4 in proliferation, migration, drug sensitivity, and stemness maintenance of pancreatic cancer cellsShi, Wang, Zhao
et alWorld J Clin Oncol (2025) 16 (3), 100723
Abstract: Pancreatic cancer (PC) is one of the most aggressive malignancies characterized by rapid progression and poor prognosis. The involvement of cancer stem cells (CSCs) and Octamer transcription factor 4 (OCT4) in PC pathobiology is being increasingly recognized.To investigate the role of OCT4 in pancreatic CSCs and its effect on PC cell proliferation, migration, drug sensitivity, and stemness maintenance.We analyzed OCT4 and CD133 expression in PC tissues and cell lines. BxPC-3 cells were used to assess the effects of OCT4 modulation on cellular behavior. Proliferation, migration, and stemness of BxPC-3 cells were evaluated, and the PI3K/AKT/mTOR pathway was examined to gain mechanistic insights.OCT4 and CD133 were significantly overexpressed in PC tissues. OCT4 modulation altered BxPC-3 cell proliferation, invasion, and stemness, with OCT4 overexpression (OV-OCT4) enhancing these properties and OCT4 interference decreasing them. OV-OCT4 activated the PI3K/AKT/mTOR pathway, which correlated with an increase in PC stem cells (PCSC).OCT4 plays a crucial role in PCSCs by influencing the aggressiveness and drug resistance of PC cells, thus presenting itself as a potential therapeutic target.©The Author(s) 2025. Published by Baishideng Publishing Group Inc. All rights reserved.
CD271 Serves as a Marker for Tumor-Initiating Cells in LaryngocarcinomaShen, Xu, Liu
et alDiscov Med (2025) 37 (194), 542-553
Abstract: Tumor-initiating cells (TICs) play a pivotal role in the unfavorable outcomes of laryngeal tumor proliferation, recurrence, and resistance to chemoradiotherapy. This study aims to explore the expression of CD271 (p75 neurotrophin receptor (p75NTR) in human laryngocarcinoma Hep2 cells and unravel its potential biological functions as a marker of laryngeal TICs.Immunomagnetic cell sorting was utilized to separate subsets of Hep-2 cells based on high and low expression levels of CD271. Various aspects such as proliferation activity, colony formation ability, cell cycle distribution, and the expression of cancer-related proteins in each subpopulation were evaluated using immunofluorescence, 3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide (MTT) assay, soft agar gel assay, flow cytometry, and western blot assay. Furthermore, the tumor-forming potential of the subsets displaying high and low CD271 expression was examined through an in vivo experiment involving nude mice. The proteins associated with the phosphorylated signal transducer and activator of transcription 3 (p-STAT3)/Octamer-binding transcription factor 4 (OCT4) pathway were detected via western blot assay.The expression of CD133 was the highest in the CD271 high-expression group, and the expression of CD133 was the lowest in the CD271 low-expression group. Hep2 cells with high CD271 expression exhibited enhanced proliferation capacity, in contrast to those with low CD271 expression which showed reduced proliferation (p < 0.05). The CD271 high-expression group of Hep2 cells demonstrated superior clonogenic ability, a higher proportion in the S and G2/M phases of the cell cycle, and an increased sphere-forming capacity. Moreover, Hep2 cells with high CD271 expression displayed enhanced tumor formation capability in nude mice (p < 0.001). Western blot analysis indicated significantly elevated levels of specific proteins such as OCT4, Nanog Homeobox (NANOG) and p-STAT3/STAT3 in the CD271 high-expression group were significantly higher than those in the control group (p < 0.01), and the protein levels of low-expression group were significantly lower than those in the control group (p < 0.01).CD271 serves as a marker for TICs in Hep-2 cells, presenting a novel target for further investigation.
Loss of TNFRSF21 induces cisplatin sensitivity in lung adenocarcinomaZhou, Yuan, Hu
et alOncol Res (2025) 33 (3), 653-663
Abstract: Despite the identification of numerous therapeutic targets in lung cancer, achieving significant efficacy has been challenging. TNFRSF21 plays an important role in various cancers. We investigated the function of TNFRSF21 in lung adenocarcinoma (LUAD).The prognostic value of TNFRSF21 expression in lung cancer was evaluated by the GEPIA and Kaplan-Meier Plotter databases. Lung cancer cell viability was assessed by the CCK8 assay. TNFRSF21 expression patterns in lung cancer tissues and cells were examined using RT-PCR assay. Tumor sphere growth was evaluated through tumor sphere formation assays. MtROS contents in lung cancer cells were observed through MitoSOX fluorescent assays.TNFRSF21 was up-regulated in LUAD patients. TNFRSF21 induction was particularly notable in LUAD, especially in cancerous cells (A549, H1299, H460, and SPC-A1), compared to BEAS-2B cells. Additionally, TNFRSF21 was increased in cisplatin (DDP)-resistant LUAD cells. Loss of TNFRSF21 significantly inhibited LUAD cell growth. It was observed that forced expression of TNFRSF21 contributed to tumor cell proliferation and DDP resistance. The production of ROS was found to participate in the inhibitory effects on lung cancer stem cells (CSCs), with decreased TNFRSF21 restraining ROS contents. Collectively, these findings reveal that the downregulation of TNFRSF21 promotes ROS contents to restrain the lung CSC-like characteristics via modulation of CD44 and CD133.In conclusion, TNFRSF21 may act as a novel target for lung cancer chemotherapy, particularly for eradicating lung CSCs.© 2025 The Author.























































 膜杰作
膜杰作 Star Staining
Star Staining















