Vitamin D stimulates Il-15 synthesis in rodent muscleEwendt, Drewitz, Althammer
et alBiochem Biophys Rep (2025) 41, 101925
Abstract: Besides its classical skeletal function, vitamin D plays a critical role in both skeletal muscle and the immune system. Interleukin-15 (IL-15), which is highly expressed, and secreted complexed with its receptor, IL-15Rα, by skeletal muscle, stimulates the development of immune cells and affects myogenesis and muscle mass. However, little is known about possible regulators of this myokine. To test whether vitamin D could be a regulator of muscle IL-15 and IL-15Rα expression, C2C12 myotubes were treated with vitamin D3 metabolites and analysis were performed in gastrocnemius muscles of rats treated with a single intraperitoneal dose of 1,25(OH)2D3. The role of VDR was investigated by siRNA technique in C2C12 myotubes and in gastrocnemius muscles of vitamin D receptor knockout (Vdr-KO) mice. Treatment of C2C12 myotubes with 1,25(OH)2D3 or 25(OH)D3 increased Il-15 gene expression in a dose-dependent manner and 1,25(OH)2D3 also moderately increased the relative Il-15 protein amount. Rats treated with a single dose of 1,25(OH)2D3 demonstrated a higher mRNA abundance of muscle Il-15 than controls. The 1,25(OH)2D3 effect on Il-15 was considerably weaker in C2C12 myotubes treated with Vdr-specific siRNA. Vdr-KO mice showed significantly lower muscle Il-15 mRNA than WT mice. Il-15Ra mRNA and Il-15/Il-15Rα protein abundance were unaffected by 1,25(OH)2D3-treatment or VDR functionality, and Cyp27b1 activity is not required for 25(OH)D3-mediated Il-15 gene expression. The results provide evidence for a regulatory role of hydroxyvitamin D3 metabolites on the Il-15 synthesis in skeletal muscle cells, which is largely mediated by the VDR.© 2025 The Authors.
Deciphering genetic causality between plasma BDNF and 91 circulating inflammatory proteins through bidirectional mendelian randomizationSun, Shi, Ohm
et alSci Rep (2025) 15 (1), 10312
Abstract: Prior studies reported an association between the levels of brain-derived neurotrophic factor (BDNF) circulating in the bloodstream and those of different inflammatory factors. However, their causal relationship remains unclear. Here, we performed a Mendelian randomization (MR) study to investigate the causal relationships between plasma BDNF levels and 91 circulating inflammatory proteins to shed light on the possible role of BDNF in the pathogenesis and progression of inflammation-related neurological diseases in order to distinguish correlation from possible causal effects. Data for plasma BDNF levels were derived from a genome-wide association study (GWAS) encompassing 3,301 European participants. Genetic association estimates for 91 inflammation proteins were extracted from a GWAS meta-analysis that enrolled 14,824 European participants. The primary MR analysis employed the inverse variance weighted (IVW) method and was corroborated by additional methods including MR-Egger, weighted median, weighted mode, and simple mode. Analyses of sensitivity were performed by evaluating the heterogeneity, horizontal pleiotropy, and robustness of the results. Genetic evidence indicated that elevated plasma BDNF levels possibly contribute to decreased concentrations of 13 inflammation proteins (OR: 0.951-0.977), including beta-nerve growth factor (Beta-NGF), caspase 8 (CASP-8), interleukin-15 receptor subunit alpha (IL-15RA), interleukin-17 A (IL-17 A), interleukin-17 C (IL-17 C), interleukin-2 (IL-2), interleukin-20 (IL-20), interleukin-20 receptor subunit alpha (IL-20RA), interleukin-24 (IL-24), interleukin-33 (IL-33), leukemia inhibitory factor (LIF), neurturin (NRTN), as well as neurotrophin-3 (NT-3). The associations between BDNF and IL-33 remained statistically significant after FDR correction (FDR > 0.05). Furthermore, reverse MR analysis showed that C-C motif chemokine 23 (CCL23), CUB domain-containing protein 1 (CDCP1), and NRTN is suggestive for a positive causal effect on BDNF plasma levels (OR: 1.240-1.422). Moreover, 5 proteins are likely to be associated with lower plasma levels of BDNF (OR: 0.742-0.971), including adenosine deaminase (ADA), cystatin D (CST5), interleukin-13 (IL-13), interleukin-17 A (IL-17 A), and vascular endothelial growth factor A (VEGF-A). Genetically determined plasma BDNF levels influence IL-33 and are possibly associated with 12 circulating inflammatory proteins. The data suggest that 8 inflammatory proteins exhibit either negative or protective roles to BDNF levels, respectively. Of these, 5 are negatively associated with BDNF levels, while 3 play protective roles. These findings may offer new theoretical and empirical insights into the pathogenesis and progression of inflammation-related neurological diseases.© 2025. The Author(s).
IL-15 transpresentation by ovarian cancer cells improves CD34+ progenitor-derived NK cell's anti-tumor functionalityVidal-Manrique, Nieuwenstein, Hooijmaijers
et alOncoimmunology (2025) 14 (1), 2465010
Abstract: Ovarian cancer (OC) is the most lethal gynecological malignancy. As high numbers of Natural Killer (NK) cells in ascites associate with improved survival, the adoptive transfer of allogeneic NK cells is an attractive therapeutic strategy. An approach to further improve NK cell expansion and anti-tumor functionality post-infusion includes IL-15 transpresentation (transIL-15), which involves surface expression of the IL-15 cytokine bound to IL-15Rα. However, others have substantiated that systemic administration of ALT/N-803, a soluble molecule mimicking transIL-15, leads to T cell-mediated rejection of the infused allogeneic NK cell product. In addition, whether transIL-15 induce superior expansion and functionality of our hematopoietic progenitor cell-derived NK cells (HPC-NK) remains understudied. Here, we propose to transfect OC cells with IL-15 and IL-15Rα mRNA and evaluate HPC-NK cell stimulation in vitro. Co-transfection of both mRNAs resulted in surface co-expression of both components, thus mimicking the transIL-15. Importantly, co-culture of HPC-NK cells with transIL-15 OC cells resulted in superior proliferation, IFNγ production, cytotoxicity and granzyme B secretion. Furthermore, we observed uptake of IL-15Rα by HPC-NK cells when co-cultured with transIL-15 OC cells, which associates with NK cell long-term proliferation and survival. Superior killing and granzyme B secretion were also observed in transIL-15 OC spheroids. Our results demonstrate that local delivery of IL-15 and IL-15Rα mRNA to OC tumors may be a safer strategy to boost HPC-NK cell therapy of OC through IL-15 transpresentation.
Causal relationship between inflammatory cytokines and polycystic ovary syndrome: a bidirectional mendelian randomization studyTian, Chen, Liu
J Ovarian Res (2024) 17 (1), 217
Abstract: Polycystic ovary syndrome (PCOS) is defined as a chronic low-grade inflammatory reproductive endocrine disorder. PCOS can induce various metabolic disorders, which are associated with a state of mild and slow-acting inflammation. Nevertheless, the causal relationship between polycystic ovary syndrome and inflammatory factors is uncertain. The causality between inflammatory cytokines and PCOS was analyzed by bidirectional Mendelian randomization (MR) in this current probe. We performed an interactive MR study to assess the causal relationships between 91 inflammatory cytokines and PCOS using Genome Wide Association Study (GWAS) data. We underwent dual-sample MR analysis with inverse variance weights (IVW) as the predominant MR methodology with multiple validity and heterogeneity analyses. MR-Egger, weighted median, simple mode, weighted mode and MR-PRESSO were analyzed as multiple likelihood sensitivity analyses to enhance the final results.The results came out interleukin-1-alpha (IL-1 A) levels (odds ratio [OR] = 1.051, 95% fiducial interval [95% CI] = 1.009-1.095, P = 0.02) and oncostatin-M (OSM) levels ( [OR] = 1.041, [95% CI] = 1.001-1.082, P = 0.04) were positively associated with the development of PCOS. Moreover, interleukin-7 (IL-7) levels ([OR] = 0.935, [95% CI] = 0.884-0.989, P = 0.02); interleukin-15 receptor subunit alpha (IL15RA) levels ([OR] = 0.959, [95% CI] = 0.929-0.99, P = 0.01); and C-X-C motif chemokine 11 (CXCL11) levels ([OR] = 0.959, [95% CI] = 0.922-0.996. P = 0.03) were strongly negatively associated with PCOS. However, we did not find any strong positive results in the reverse analysis, suggesting that although inflammatory factors contribute to the pathogenesis of PCOS, PCOS itself does not trigger inflammatory factor production.Our study provides genetic evidence for the connection between systemic inflammatory regulators and PCOS. Treatments targeting specific inflammatory factors may help to mitigate the risk of PCOS. The levels of five of the 91 inflammatory factors included in this study, namely, IL1A and OSM, were associated with PCOS. IL1A and OSM contribute to the progression of PCOS while IL-7, IL15RA, and CXCL11 levels are negatively correlated with the development of PCOS.© 2024. The Author(s).
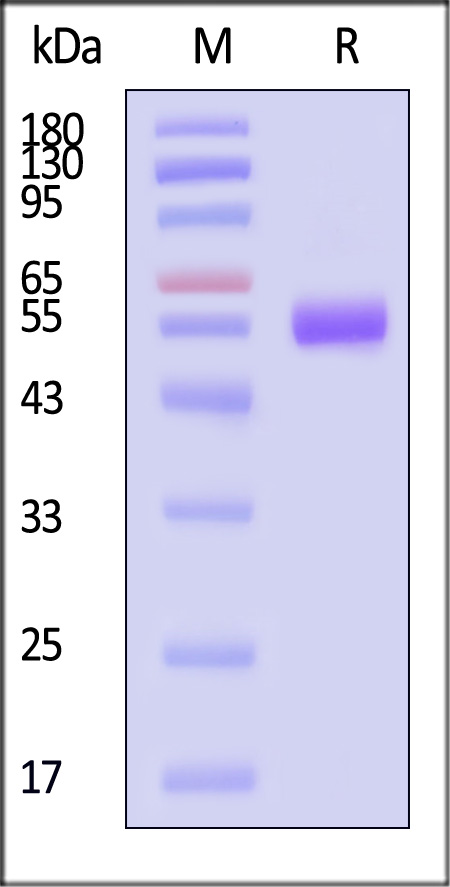
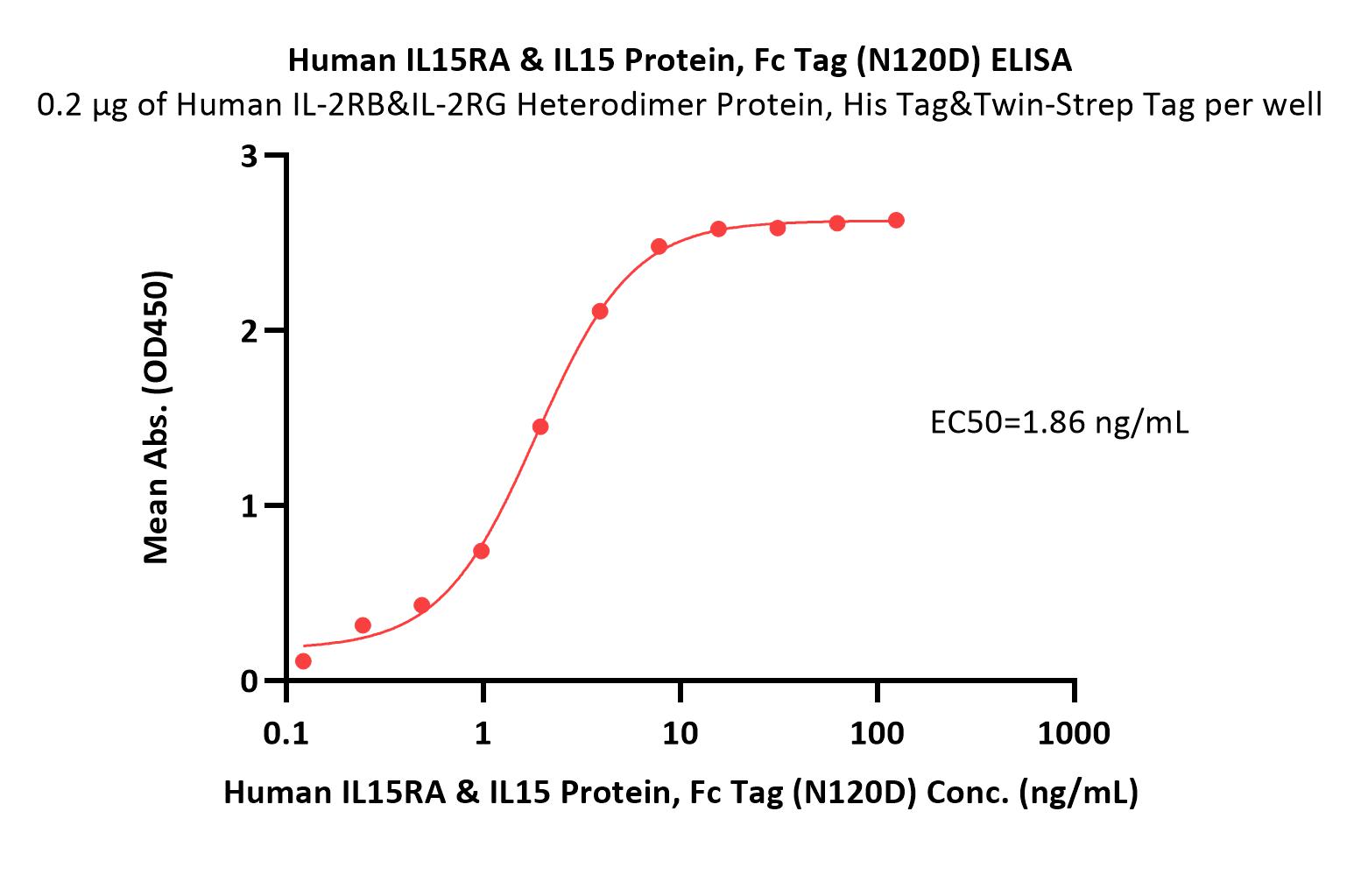















































 膜杰作
膜杰作 Star Staining
Star Staining