PVR exposure influences the activation, adhesion, and protein expression of human CD8+ T cells, including the CD96-mediated transfer of PVRHuang, Pawge, Snicer
et alJ Immunol (2025) 214 (1), 55-71
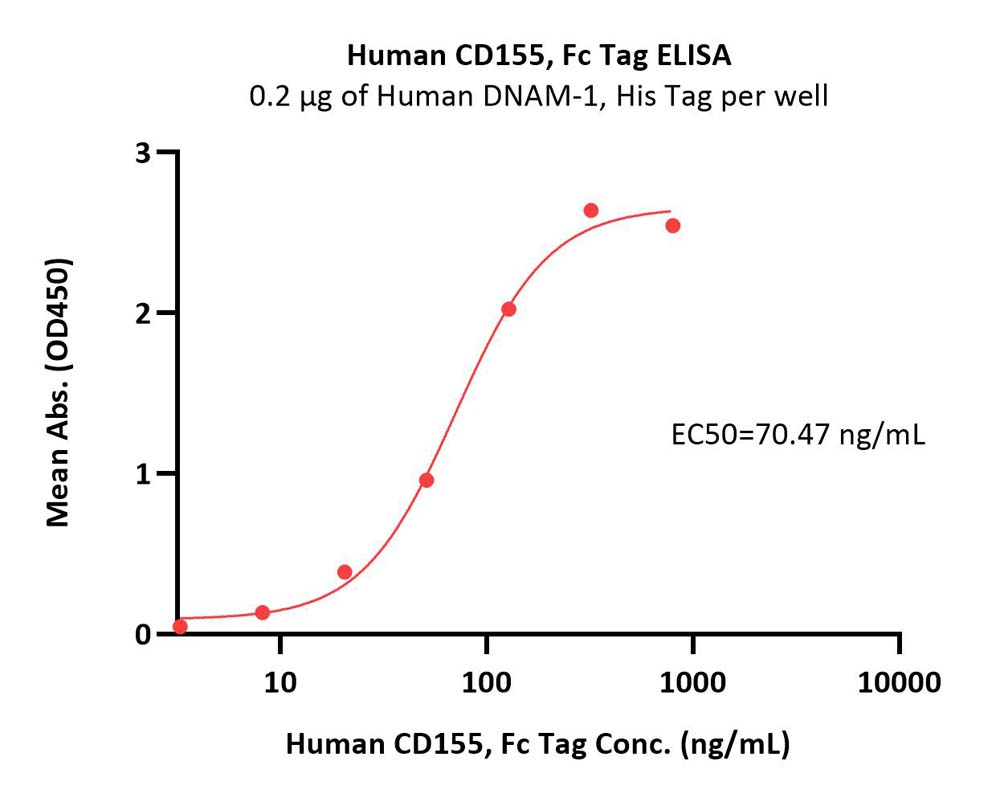
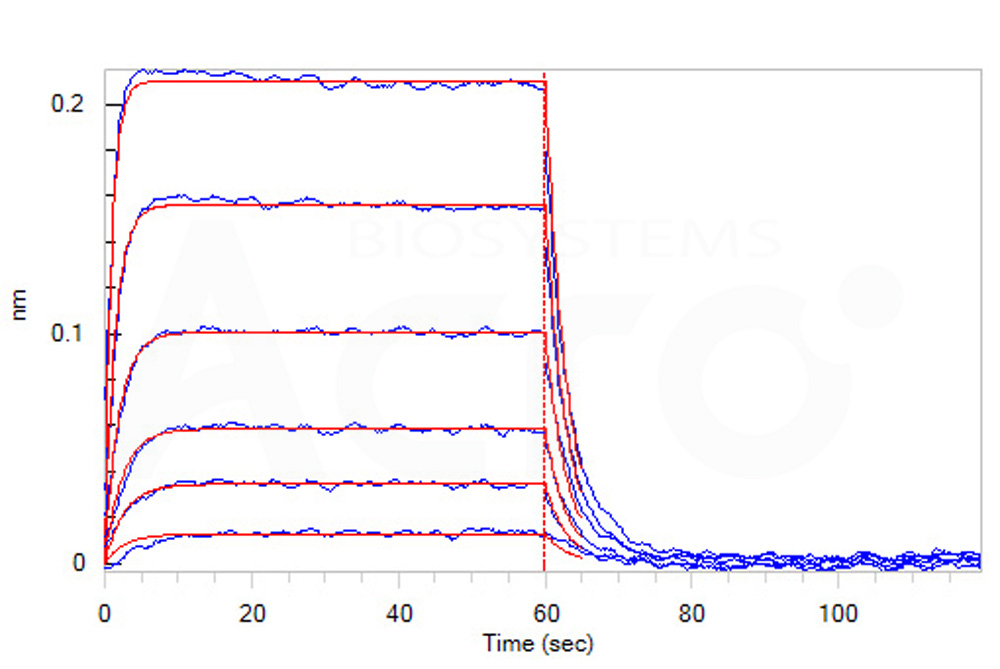
Abstract: Poliovirus receptor (PVR) ligands have gained attention as immunotherapy targets, yet their regulation remains unclear. Here, we examine the impact of PVR exposure on primary human CD8+ T cells. We used flow cytometry and Western blot analysis to quantify expression of PVR and its ligands in naïve and effector T cells and used adhesion assays and enzyme-linked immunosorbent assay (ELISA) to assess the impact of PVR on T cell adhesion and cytokine production. Stimulation with phytohemagglutinin P strongly increased DNAM-1 expression and caused a less robust and more variable increase in TIGIT expression. Exposure to PVR-Fc enhanced the CD8+ T cell adhesion to ICAM-1-coated plates in a dose-dependent manner, while exposure to PVR-expressing K32 cells mildly decreased CD8+ T cell interferon γ release. However, PVR exposure strongly decreased the expression of DNAM-1, TIGIT, and CD96. The reduction of DNAM-1, TIGIT, and CD96 induced by PVR was dominant to the increase caused by T cell receptor signaling. The impact of PVR on their expression was completely abolished by the Q63R and F128R point mutations of PVR, while DNAM-1 was partially rescued by inhibitors of Src and protein kinase C. Additionally, PVR exposure along with T cell receptor signaling promoted the transfer of surface proteins including PVR from K32 cells to CD8+ T cells. This PVR transfer was mediated by the IgV domain of PVR and CD96 on CD8+ T cells and required cellular contact. Our findings collectively demonstrate that PVR engagement has a mild antagonistic effect on interferon γ production but strongly impacts CD8+ T cell adhesion and protein expression.© The Author(s) 2025. Published by Oxford University Press on behalf of The American Association of Immunologists.
A chimeric antigen receptor tailored to integrate complementary activation signals potentiates the antitumor activity of NK cellsYi, Lee, Park
et alJ Exp Clin Cancer Res (2025) 44 (1), 86
Abstract: Chimeric antigen receptors (CARs) are synthetic receptors that reprogram the target specificity and functions of CAR-expressing effector cells. The design of CAR constructs typically includes an extracellular antigen-binding moiety, hinge (H), transmembrane (TM), and intracellular signaling domains. Conventional CAR constructs are primarily designed for T cells but have been directly adopted for other effector cells, including natural killer (NK) cells, without tailored optimization. Given the benefits of CAR-NK cells over CAR-T cells in terms of safety, off-the-shelf utility, and antigen escape, there is an increasing emphasis on tailoring them to NK cell activation mechanisms.We first have taken a stepwise approach to modifying CAR components such as the combination and order of the H, TM, and signaling domains to achieve such tailoring in NK cells. Functionality of NK-tailored CARs were evaluated in vitro and in vivo in a model of CD19-expressing lymphoma, along with their expression and signaling properties in NK cells.We found that NK-CAR driven by the synergistic combination of NK receptors NKG2D and 2B4 rather than DNAM-1 and 2B4 induces potent activation in NK cells. Further, more effective CAR-mediated cytotoxicity was observed following the sequential combination of DAP10, but not NKG2D TM, with 2B4 signaling domain despite the capacity of NKG2D TM to recruit endogenous DAP10 for signaling. Accordingly, an NK-CAR incorporating DAP10, 2B4, and CD3ζ signaling domains coupled to CD8α H and CD28 TM domains was identified as the most promising candidate to improve CAR-mediated cytotoxicity. This NK-tailored CAR provided more potent antitumor activity than a conventional T-CAR when delivered to NK cells both in vitro and in vivo.Hence, NK receptor-based domains hold great promise for the future of NK-CAR design with potentially significant therapeutic benefits.© 2025. The Author(s).
Multiple Myeloma Cells Shift the Fate of Cytolytic ILC2s Towards TIGIT-Mediated Cell DeathDrommi, Calabrò, Pezzino
et alCancers (Basel) (2025) 17 (2)
Abstract: Growing evidence attests to the multifaceted roles of group 2 innate lymphoid cells (ILC2s) in cancer immunity. They exhibit either pro- or anticancer activity depending on tumor type but their function in Multiple Myeloma (MM) is still not elucidated.The bone marrow (BM) and peripheral blood (PB) of patients (pts) with MM or precancerous conditions were collected, and specific properties of ILC2 subsets were assessed by flow cytometry.By dissecting ILC2s according to c-Kit marker, we observed that NKp30 and NKG2D were mainly confined to c-Kithi ILC2s, while levels of DNAM-1 was significantly higher in fully mature c-Kitlo cells. Among the total MM-associated ILC2s (MM-ILC2s), we observed a significant increase in c-the Kitlo subset, but the expression of DNAM-1 in these cells was significantly reduced, especially in BM. Interestingly, MM-ILC2s from PB expressed granzyme B (GZMB), but its expression was impaired in BM-ILC2s. Accordingly, MM cells were susceptible to killing by MM-ILC2s derived from PB while eluding ILC2 surveillance in BM. Indeed, in MM-ILC2s derived from BM, the downregulation of DNAM-1 is accompanied by the upregulation of TIGIT, which mediate cell death in ILC2s upon recognition of the cognate ligands expressed by MM cells. These ILC2 changes appeared in clinical precursor conditions and eventually accumulated with disease progression.MM-ILC2s can act as cytolytic immune effectors that are fully competent in PB. However, MM cells shift ILC2 fate towards cell death in BM via the upregulation of TIGIT, thereby representing a potential therapeutic target to restore ILC2 antitumor activity.
The emergence of DNAM-1 as the facilitator of NK cell-mediated killing in ovarian cancerPounds, Croft, Pearce
et alFront Immunol (2024) 15, 1477781
Abstract: Ovarian cancer (OC) is the sixth most common malignancy in women and the poor 5-year survival emphasises the need for novel therapies. NK cells play an important role in the control of malignant disease but the nature of tumour-infiltrating and peripheral NK cells in OC remains unclear.Using flow cytometric analysis, we studied the phenotype and function of NK cells in blood, primary tumour and metastatic tissue in 80 women with OC. The cell type contexture of metastatic OC tissue was explored utilising scRNAseq analysis, with a focus on portraying an immunogenic tumour microenvironment and determining the characteristics of a dysfunctional NK cell population.The proportion of peripheral NK cells was markedly elevated with a highly activated profile and increased cytotoxicity. In contrast, NK cell numbers in primary tumour and metastasis were substantially reduced, with downregulation of activatory receptors together with elevated PD-1 expression. scRNA-Seq identified 5 NK cell subpopulations along with increased exhausted and immature NK cells within tumour tissue compared to normal tissue. These features were attenuated following chemotherapy where higher levels of activated and cytotoxic NK cells associated with improved disease-free survival. Correlation of NK cell phenotype with clinical outcomes revealed high levels of DNAM-1 expression on tissue-localised and peripheral NK cells to be associated with reduced survival. Expression of PVR, the DNAM-1 ligand, was significantly increased on tumours and DNAM-1 mediated NK cell lysis of primary tumour tissue was observed in vitro.These findings reveal profound modulation of the tumour tissue and systemic profile of NK cells which likely contributes to the high rates of local progression and metastasis seen with OC. Immunotherapeutic approaches that overcome local immune suppression and enhance DNAM-1-targeted lysis of OC offer the potential to improve disease control.Copyright © 2025 Pounds, Croft, Pearce, Hossain, Singh, Balega, Jeevan, Sundar, Kehoe, Yap, Moss and Zuo.























































 膜杰作
膜杰作 Star Staining
Star Staining
















