Fibroblast growth factor receptor signaling in metabolic dysfunction-associated fatty liver disease: Pathogenesis and therapeutic targetsChu, Yang, Chen
Pharmacol Ther (2025) 269, 108844
Abstract: Metabolic dysfunction-associated fatty liver disease (MAFLD) has emerged as a significant hepatic manifestation of metabolic syndrome, with its prevalence increasing globally alongside the epidemics of obesity and diabetes. MAFLD represents a continuum of liver damage, spanning from uncomplicated steatosis to metabolic dysfunction-associated steatohepatitis (MASH). This condition can advance to more severe outcomes, including fibrosis and cirrhosis. Fibroblast growth factor receptors (FGFRs) are a family of four receptor tyrosine kinases (FGFR1-4) that interact with both paracrine and endocrine fibroblast growth factors (FGFs). This interaction activates the phosphorylation of tyrosine kinase residues, thereby triggering downstream signaling pathways, including RAS-MAPK, JAK-STAT, PI3K-AKT, and PLCγ. In the context of MAFLD, paracrine FGF-FGFR signaling is predominantly biased toward the development of liver fibrosis and carcinogenesis. In contrast, endocrine FGF-FGFR signaling is primarily biased toward regulating the metabolism of bile acids, carbohydrates, lipids, and phosphate, as well as maintaining the overall balance of energy metabolism in the body. The interplay between these biased signaling pathways significantly influences the progression of MAFLD. This review explores the critical functions of FGFR signaling in MAFLD from three perspectives: first, it examines the primary roles of FGFRs relative to their structure; second, it summarizes FGFR signaling in hepatic lipid metabolism, elucidating mechanisms underlying the occurrence and progression of MAFLD; finally, it highlights recent advancements in drug development aimed at targeting FGFR signaling for the treatment of MAFLD and its associated diseases.Copyright © 2025 Elsevier Inc. All rights reserved.
Bile acid receptor FXR promotes intestinal epithelial ferroptosis and subsequent ILC3 dysfunction in neonatal necrotizing enterocolitisZhang, Jing, He
et alImmunity (2025) 58 (3), 683-700.e10
Abstract: Necrotizing enterocolitis (NEC) is a common pediatric emergency primarily afflicting preterm infants, yet its mechanisms remain to be fully understood. Here, we report that plasma fibroblast growth factor (FGF)19, a target of farnesoid X receptor (FXR), was positively correlated with the clinical parameters of NEC. NEC patients and the NEC murine model displayed abundant FXR in intestinal epithelial cells (IECs), which was restricted by microbiota-derived short-chain fatty acids (SCFAs) under homeostasis. Genetic deficiency of FXR in IECs caused remission of NEC. Mechanistically, FXR facilitated ferroptosis of IECs via targeting acyl-coenzyme A synthetase long-chain family member 4 (Acsl4). Lipid peroxides released by ferroptotic IECs suppressed interleukin (IL)-22 secretion from type 3 innate lymphoid cells (ILC3s), thereby exacerbating NEC. Intestinal FXR antagonist, ACSL4 inhibitor, and ferroptosis inhibitor ameliorated murine NEC. Furthermore, the elevated lipid peroxides in NEC patients were positively correlated with FGF19 and disease parameters. These observations demonstrate the therapeutic value of targeting intestinal FXR and ferroptosis in NEC treatment.Copyright © 2025 Elsevier Inc. All rights reserved.
Factors associated with phosphate homeostasis in children with beta-thalassemia major: An analytical cross sectional study from PakistanJafri, Jameel Farooqui, Moiz
et alPLoS One (2025) 20 (2), e0316566
Abstract: Children with beta-thalassemia major (β-TM) commonly experience metabolic bone diseases. Understanding fibroblast growth factor 23 (FGF-23) levels in these children can shed light on phosphate dysregulation. This study aimed to assess changes in phosphate homeostasis and associated factors, including FGF-23 and explore relationships between iron overload, FGF23 levels, and phosphorus regulation for clinical management of phosphate disorders, in children with β-TM.143 β-TM patients (57.3% male, median age 12 years) were recruited from Fatimid Foundation Karachi, a blood transfusion facility from January to October 2022. Clinical and biochemical evaluations were conducted at Aga Khan University Hospital, including serum ferritin, calcium (Ca), phosphate (P), vitamin D levels, and FGF-23. Descriptive and inferential statistics including multivariable analysis were applied.This study enrolled 143 patients, with 57.3% males. The median age was 12 years, with 53% underweight. Blood transfusion rates varied, with 66.4% receiving 2/month. Bone/joint pain was reported by 76.2%, with 60.8% requiring analgesics. Median serum ferritin was 2768.3 ng/mL. Hypophosphatemia and hyperphosphatemia were observed in 5.6% and 3.5% of participants, respectively. Vitamin D deficiency/insufficiency affected 92.3%. Plasma c-FGF23 was elevated in 60.8%, while i-FGF23 was high in 14%. A low TMP-GFR (glomerular filtration rate) was associated with high c-FGF23 and low i-FGF23. Multivariable regression revealed c-FGF23, TMP:GFR, Corrected Ca, iPTH, and an interaction term between corrected Ca and iPTH as predictors of serum P variability (~75%).The study identified contributors to the variations observed in serum P levels in individuals with β-TM and recommends multidisciplinary care and prospective future studies to form targeted interventions for this population.Copyright: © 2025 Jafri et al. This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
[Rare osteological diseases in the rheumatological consultation: hypophosphatasia and phosphate loss syndromes]Bauer, Schäfer, Boyadzhieva
et alZ Rheumatol (2025) 84 (2), 128-137
Abstract: Metabolic bone diseases cause bone and joint pain and are manifested as rheumatism. Typical for the rare genetic disease hypophosphatasia is a reduced activity of alkaline phosphatase (AP), where the variable residual activity causes the heterogeneous symptoms (e.g., arthralgia, myalgia and fractures). It is indicated by repeatedly low AP measurements. The diagnosis requires a meticulous medical history and laboratory-based clarification in order to rule out other differential diagnoses. Although supportive measures form the basis of treatment, costly enzyme replacement therapy is a possible treatment option for severe forms. Multidisciplinary care under the direction of a rheumatologist experienced in osteology or an osteologist is crucial in order to provide adequate care to affected patients. Phosphate loss syndromes due to overactivity of fibroblast growth factor 23 (FGF-23) lead to deformities of the lower extremities and short stature (in congenital disorders), bone and muscle pain, muscular weakness and pathological fractures, depending on the time of occurrence during life. In genetic forms of the disease (especially X‑linked hypophosphatemia), supplementation with calcitriol and phosphates and, if necessary, complex corrective surgery in adolescence are traditional treatment methods, which are increasingly being replaced by treatment with antibodies against FGF-23. The acquired variant is a paraneoplastic phenomenon from small mostly benign mesenchymal tumors, which clinically shows a relatively acute course with severe bone pain, pathological fractures and muscle weakness in previously healthy patients and can ideally be cured by resection of the tumor. The disease can be suspected by significantly reduced serum phosphate levels and narrowed down with further laboratory diagnostics. In our opinion, the measurement of calcium, phosphate and alkaline phosphatase should be part of the primary laboratory diagnostics performed by rheumatologists and the follow-up of pathological findings is indicated.© 2025. The Author(s), under exclusive licence to Springer Medizin Verlag GmbH, ein Teil von Springer Nature.

 +添加评论
+添加评论
 >
>






















































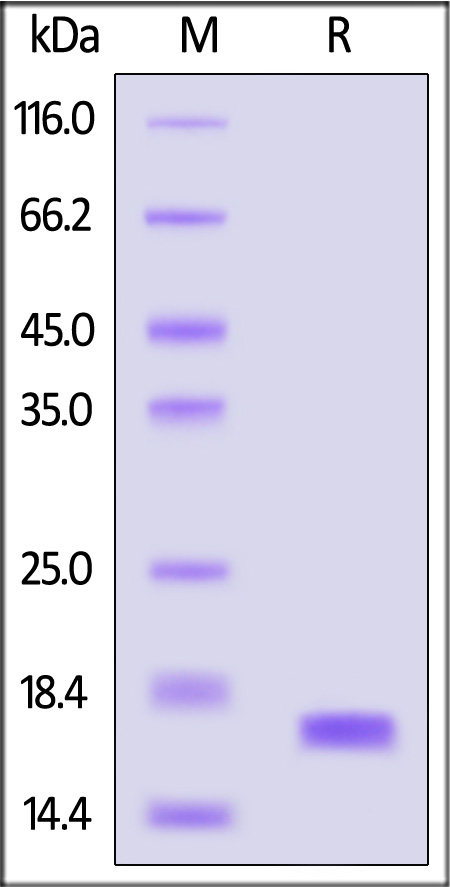
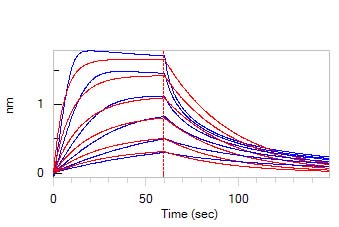
 膜杰作
膜杰作 Star Staining
Star Staining