Synovial fluid glycoproteome profiling in knee osteoarthritis: Molecular insights into type 2 diabetes-associated biomarkers and therapeutic targetsKonar, Kaur, Saini
et alBiochim Biophys Acta Proteins Proteom (2025)
Abstract: Type 2 diabetes mellitus (T2DM) and osteoarthritis (OA) share common risk factors like age, obesity and hypertension. Currently, 52 % of diabetic patients suffer from arthritis. Diabetes facilitates osteoarthritis by altering lipid metabolism, levels of adipokines & cytokines, accumulation of advanced glycation end products, etc. which affects cartilage & bone health. However, the molecular mechanisms of association of OA with T2DM remain unexplored. Since diabetes greatly affects the glycosylation status of proteins, the present study focused on identifying glycoproteins that could serve as diagnostic and prognostic markers for identifying osteoarthritis in diabetic individuals by LC-MS/MS. Comparative analysis revealed 20 significantly altered glycoproteins; among them, thyroxine-binding globulin (THBG), alpha-1-antitrypsin (A1AT), fibrinogen gamma chain (FGG) and angiotensinogen (AGT) were further validated. THBG, A1AT and ANGT showed promising potential to identify the comorbid condition in serum and synovial fluid, however, ROC analysis identified THBG as the best candidate glycoprotein marker. Upregulation of THBG in OADM disrupts the bone remodeling cycle, degrades insulin, and promotes the expression of GLUT-1 and MMP-9. Overall, THBG could also serve as a therapeutic target for reducing the progression of osteoarthritis and alleviating pain and bone stiffness associated with the disease.Copyright © 2025. Published by Elsevier B.V.
Applied physiological principles in the management of a lung allograft to thoracic cavity size mismatch in severe emphysemaEberlein, Keech, Reed
JHLT Open (2024) 6, 100124
Abstract: In this review, we discuss physiological principles that guided the management of a lung transplant for emphysema related to alpha-1-antitrypsin deficiency, where a lung allograft to thoracic cavity size mismatch occurred (donor-to-recipient predicted total lung capacity [pTLC] ratio was 0.89, donor pTLC-to-recipient actual-TLC ratio 0.62). In emphysema, the loss of lung elastic recoil and airway obstruction leads to air trapping and lung hyperinflation. Remodeling of the thoracic cavity ("barrel chest") develops, which has implications for donor-to-recipient sizing and postoperative management of lung transplantation. We discuss the physiology of a relatively undersized allograft and the impact on chest tube, mechanical ventilation, and respiratory system mechanics management. This case also illustrates how chronic adaptations of the ventilatory pattern to advanced lung diseases are reversible and the chest cavity size can remodel back to normal after lung transplantation.© 2024 International Society for Heart and Lung Transplantation.
Lung transplant outcomes for recipients with alpha-1 antitrypsin deficiency, by use of alpha-1 antitrypsin augmentation therapyOak, Ruck, Casillan
et alJHLT Open (2025) 7, 100201
Abstract: For patients with alpha-1 antitrypsin (AAT) deficiency, AAT augmentation therapy can be an important part of care. However, for those who require a lung transplant (LT), there is currently only limited information to guide the use of AAT augmentation therapy post-LT.We identified all LT recipients from 2011-2021 in the Scientific Registry of Transplant Recipients with an AAT deficiency diagnosis. We categorized recipients by use of AAT augmentation therapy post-LT and compared their baseline characteristics using Fisher's exact test and Wilcoxon rank-sum tests. We used Kaplan-Meier analyses and estimated the average treatment effect (ATE) of post-LT AAT augmentation therapy on mortality and all-cause graft failure (ACGF). The ATE measures the observed effect we would see if everyone in the population received the intervention as opposed to just a subset.Among the 447 recipients with AAT deficiency, 109 used AAT augmentation therapy pre-LT, of which 32 (29.4%) continued post-LT. Recipients who used augmentation therapy post-LT were younger (56.5 [53-59.75] vs 57 [53.75-63], p = 0.04) and had shorter ischemia time (mean 311 vs 363 minutes, p = 0.03) than those who did not. The age-adjusted ATE estimate of post-LT augmentation therapy use on time to death and ACGF was +1.69 and +1.48 years, respectively. Post-LT augmentation therapy use was associated with a mortality reduction in the top quartile bilirubin subgroup (p = 0.02, log-rank test).In our study, the use of augmentation therapy post-LT was associated with improved survival. Confirmatory prospective studies should be considered to inform post-LT AAT therapy guidelines.© 2025 International Society for Heart and Lung Transplantation.
Plasma Exosomal-Derived SERPINA1 and GNAI2 Downregulation as Potential Diagnostic Biomarkers of Kawasaki Disease with Coronary Artery AneurysmsZheng, Bai, Wei
et alInt J Mol Sci (2025) 26 (6)
Abstract: Kawasaki disease (KD) with coronary artery aneurysms (CAAs) is currently the primary cause of childhood acquired heart disease with an unclear pathogenesis. We established five groups for the discovery of differentially expressed proteins (DEPs): healthy control, febrile control, KD without CAAs, KD with small and medium CAAs, and KD with giant CAAs (n = 8 in each group). The validation of selected DEPs was conducted in another five groups (n = 4 in each group). We conducted comprehensive bioinformatics analyses to elucidate the functional roles of the DEPs in the groups of KD with CAAs and KD without CAAs. A total of 104 DEPs were identified in KD patients, which were primarily associated with complement-related pathways. A trend analysis of these 104 DEPs revealed 54 significantly changed DEPs associated with increased disease severity, which were primarily associated with G-protein-related functions. The alterations in α-1-antitrypsin short peptide (SERPINA1) and guanine nucleotide-binding protein G(i) subunit alpha-2 (GNAI2), which were selected from complement-related and G-protein-related pathways, respectively, were validated by Western blotting, and they were significantly decreased in KD patients with vs. without CAAs. In addition, we conducted an analysis of the DEPs in the groups of KD with CAAs and KD without CAAs, separately. There were 91 DEPs specifically expressed in KD patients with CAAs, associated with the neutrophil extracellular trap and complement pathways, while 16 DEPs were specific to those without CAAs, associated with viral infection and immunity pathways. Additionally, for DEPs among different severities of CAAs, there were 102 DEPs in KD patients with small and medium CAAs, associated with complement pathways and platelet activation pathways, whereas 34 DEPs were specific to giant CAAs, associated with the Rap1 signaling pathway and cell functions. In conclusion, this study provides plasmatic exosomal protein profiles in KD patients with CAAs, suggesting that SERPINA1 and GNIA2 might serve as novel potential diagnostic biomarkers for KD with CAAs.

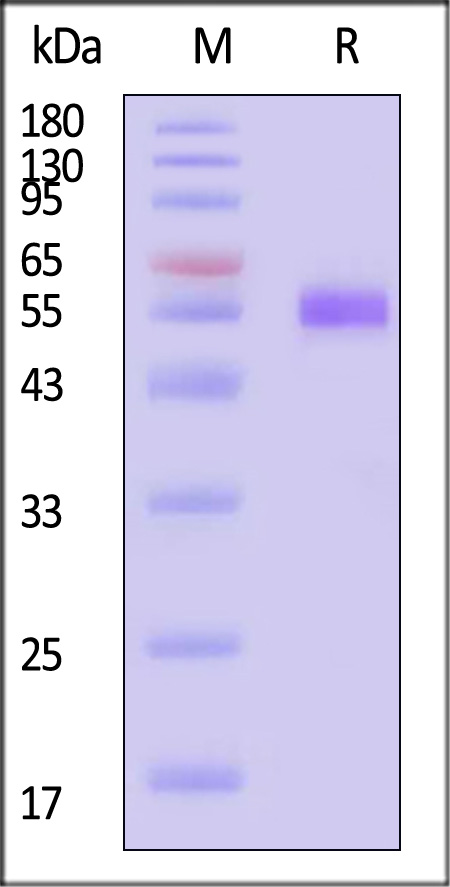























































 膜杰作
膜杰作 Star Staining
Star Staining