The NGAL as a prognostic biomarker of kidney injury in children and adolescents with type 1 diabetes mellitus: A systematic review and meta-analysisGkiourtzis, Stoimeni, Michou
et alJ Diabetes Complications (2025) 39 (5), 109002
Abstract: A major complication of type 1 diabetes is diabetic kidney disease (DKD). Albuminuria and impaired glomerular filtration rate are the main characteristics of DKD. Neutrophil gelatinase-associated lipocalin (NGAL) levels may rise even in the early stages of DKD, even in patients with normoalbuminuria. We present the first systematic review and meta-analysis examining the prognostic role of NGAL exclusively in pediatric patients with type 1 diabetes.A search through major databases was carried out until September 24, 2024, investigating the prognostic role of NGAL in kidney injury in pediatric patients with type 1 diabetes. A p < 0.05 was considered statistically significant. A study quality assessment was conducted using the Newcastle-Ottawa Scale.The standardized mean difference in urinary NGAL (uNGAL) levels between the type 1 diabetes group and healthy controls was statistically significant (SMD = 0.63, 95%CI [0.36,0.90]). A moderate positive relationship between uNGAL and ACR was identified (r = 0.53, 95 % CI [0.31-0.70]). The uNGAL revealed a high overall diagnostic accuracy (AUC = 0.881).Urinary NGAL appears to be a valuable biomarker for early detection and understanding of DKD in individuals with type 1 diabetes. Future clinical studies should prioritize assessing the accuracy of NGAL in identifying kidney injury in pediatric patients with type 1 diabetes and the association of NGAL with traditional biomarkers in groups with similar characteristics.Copyright © 2025 The Authors. Published by Elsevier Inc. All rights reserved.
Urinary biomarkers in prediction of subclinical acute kidney injury in pediatric oncology patients treated with nephrotoxic agentsMiloševski-Lomić, Kotur-Stevuljević, Paripović
et alBMC Nephrol (2025) 26 (1), 159
Abstract: Acute kidney injury (AKI) is a common complication in pediatric oncology patients, most often caused by nephrotoxic drugs. We aimed to assess whether levels of urinary kidney injury molecule-1 (uKIM-1), neutrophil gelatinase-associated lipocalin (uNGAL), liver fatty acid binding protein (uL-FABP) and Vanin-1 (uVNN-1), individually and in combination-integrated could be early markers for cytotoxic treatment induced AKI.Children with different malignant diseases treated with cisplatin (CIS) or ifosfamide (IFO) were included. AKI was defined using pediatric KDIGO (Kidney Disease Improving Global Outcomes) criteria by comparing pretreatment serum creatinine (sCr) values with those acquired at 48 h after the first or second chemotherapy cycle. Five serum (at baseline, 2, 6, 24 and 48 h after treatment) and four urine samples (at baseline, 2, 6 and 24 h after treatment) were obtained. Urinary biomarkers (uBm) were normalized to urine creatinine.Thirty-eight patients were assessed. Within 48 h following chemotherapy 6 (15.79%) patients experienced AKI. Patients with AKI were younger and tend to have lower baseline sCr values than patients without AKI, but these differences were not statistically significant. Compared to baselines, all uBm were significantly increased during the first 6 h while sCr concentrations did not change significantly during the study period. The median increases in uBm during the first 6 h after treatment were 529.8% (interquartile range - IQR, 63.9-1835.2%) - 2194.0% (IQR, 255.3-4695.5%) in AKI vs. 302.2% (IQR 114.6-561.2%) -429.8% (156.5-1467.0%) in non-AKI group depending of tested uBm. The magnitude of these changes over time didn't differ significantly between groups. The area under receiver operator curve (AUC) for uL-FABP and uNGAL at 24 h after chemotherapy were 0.81 and 0.72, respectively. The ROC analysis revealed that the other individual biomarkers' performance at any time-point wasn't statistically significant (AUC < 0.7). A model of integrated-combined uBm, 2 h (AUC 0.78), 6 h (AUC 0.85) and 24 h after (AUC 0.92) treatment with CIS and/or IFO showed good utility for early AKI prediction.The results of this study support that the use of the uBm to improves early AKI prediction in patients receiving CIS and/or IFO containing chemotherapy. Further studies on larger comparable groups of patients are needed.© 2025. The Author(s).
























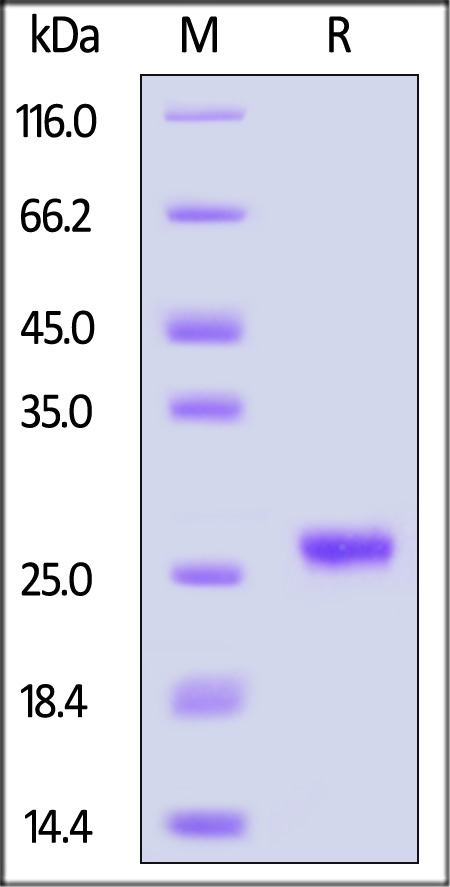
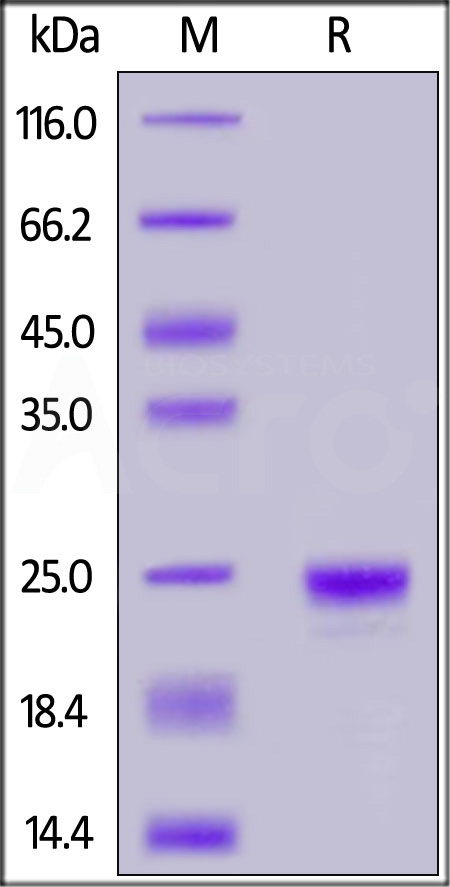
 Star Ribbon预染蛋白Marker蛋白质标记物是生物研究和药物开发的重要组成部分。无论是用于蛋白质电泳还是western blot,我们的预染色蛋白质标记物帮助您快速确定目标蛋白质的分子量或评估转移效率。Fc受体蛋白治疗性抗体的功效取决于Fab片段及其对目标抗原的结合活性,还取决于Fc片段及其与关键Fc受体的相互作用。因此,在抗体工程中候选物必须针对一系列受体进行测试。探索我们的重组Fc受体蛋白质的全面收藏!
Star Ribbon预染蛋白Marker蛋白质标记物是生物研究和药物开发的重要组成部分。无论是用于蛋白质电泳还是western blot,我们的预染色蛋白质标记物帮助您快速确定目标蛋白质的分子量或评估转移效率。Fc受体蛋白治疗性抗体的功效取决于Fab片段及其对目标抗原的结合活性,还取决于Fc片段及其与关键Fc受体的相互作用。因此,在抗体工程中候选物必须针对一系列受体进行测试。探索我们的重组Fc受体蛋白质的全面收藏!





















 膜杰作
膜杰作 Star Staining
Star Staining