Tezepelumab inhibits highly functional truncated thymic stromal lymphopoietin in chronic rhinosinusitisOka, Klingler, Kidoguchi
et alJ Allergy Clin Immunol (2025)
Abstract: Thymic stromal lymphopoietin (TSLP) and its functional cleavage products are elevated in nasal polyps (NPs) and play important roles in type 2 (T2) inflammation in chronic rhinosinusitis (CRS) with nasal polyps (CRSwNP) by activating myeloid dendritic cells (mDCs) and group 2 innate lymphoid cells (ILC2s). However, whether tezepelumab, a human mAb against TSLP, inhibits functional cleaved TSLP and also the role of TSLP in CRS without nasal polyps (CRSsNP) have not yet been studied.We sought to investigate the effects of tezepelumab on cleaved TSLP in CRS.The mRNA expression levels for TSLP and T2 markers in ethmoid tissues (ETs) from 31 controls and 118 patients with CRSsNP and in NPs from 53 patients with CRSwNP were measured by quantitative RT-PCR. Cleaved TSLP was prepared from full-length recombinant TSLP by incubation with tissue extracts of NPs and CRSsNP ETs. The effects of tezepelumab on cleaved TSLP-induced inflammation were evaluated using PBMCs by monitoring the production of chemokines (CCL17 and CCL22 for mDCs) and cytokines (IL-5 and IL-13 for ILC2s).The mRNA expression level of TSLP was elevated not only in NPs but also in ETs from T2 CRSsNP compared with non-T2 CRSsNP and controls, and was positively correlated with T2 markers in CRSsNP (P < .001). CRSsNP ET also truncated and created highly active TSLP products. The activation of mDCs and ILC2s by full-length TSLP and cleaved TSLP created by ET and NP extracts was dose-dependently inhibited by tezepelumab.TSLP plays a role in T2 inflammation in CRSsNP and CRSwNP. Treatment with tezepelumab may benefit patients with T2 CRS by inhibiting active forms of TSLP.Copyright © 2025 American Academy of Allergy, Asthma & Immunology. Published by Elsevier Inc. All rights reserved.
Enhanced Siglec-8 and HLA-DR and Reduced CRTH2 Surface Expression, Highlight a Distinct Phenotypic Signature of Circulating Eosinophils in Atopic DermatitisDezoteux, Marcant, Dendooven
et alJ Leukoc Biol (2025)
Abstract: Atopic dermatitis (AD) as well as other type 2 immune response (T2) diseases are often linked to elevated eosinophil (Eos) levels in the blood. Although the role of Eos in AD pathophysiology is suspected, it remains unclear. The development of new treatments targeting the T2 response, particularly cytokines involved in Eos activation and chemotaxis, makes it necessary to identify potential Eos profiles in AD that may respond to these treatments. A prospective study was conducted comparing blood Eos phenotypes in moderate-to-severe AD patients (n=19) without recent systemic treatment to healthy individuals (HI, n=19). The primary outcome was the membranous phenotypic signature of Eos, assessed by flow cytometry. Most AD patients (84%) had early onset in childhood, a severe disease (mean SCORAD of 57.5), and elevated blood Eos counts (310 per µl in AD vs 120 in HI, p<0.0001). AD patients exhibited lower CRTH2 on Eos but higher levels of HLA-DR and Siglec-8 compared to HI. Other surface proteins showed no significant differences. Clustering analysis confirmed increased Siglec-8 in AD patients. Additionally, AD patients had higher serum levels of T2 immune response-markers as eotaxin-2, IL-5, IL-3, and TARC. Circulating Eos in AD patients show a distinct phenotypic profile, suggesting a role in AD pathophysiology and potential involvement in differential treatment responses.© The Author(s) 2025. Published by Oxford University Press on behalf of Society for Leukocyte Biology. All rights reserved. For commercial re-use, please contact reprints@oup.com for reprints and translation rights for reprints. All other permissions can be obtained through our RightsLink service via the Permissions link on the article page on our site—for further information please contact journals.permissions@oup.com.
Understanding the Glycosylation Pathways Involved in the Biosynthesis of the Sulfated Glycan Ligands for SiglecsJung, Schmidt, Chang
et alACS Chem Biol (2025) 20 (2), 386-400
Abstract: Carbohydrate sulfation plays a pivotal role in modulating the strength of Siglec-glycan interactions. Recently, new aspects of Siglec binding to sulfated cell surface carbohydrates have been discovered, but the class of glycan presenting these sulfated Siglec ligands has not been fully elucidated. In this study, the contribution of different classes of glycans to cis and trans Siglec ligands was investigated within cells expressing the carbohydrate sulfotransferase 1 (CHST1) or CHST2. For some Siglecs, the glycan class mediating binding was clear, such as O-glycans for Siglec-7 and N-glycans for Siglec-2 and Siglec-9. Both N-glycans and mucin-type O-glycans contributed to ligands for Siglec-3, -5, -8, and -15. However, significant levels of Siglec-3 and -8 ligands remained in CHST1-expressing cells lacking complex N-glycans and mucin-type O-glycans. A combination of genetic, pharmacological, and enzymatic treatment strategies ruled out heparan sulfates and glycoRNA as contributors, although Siglec-8 did exhibit some binding to glycolipids. Genetic disruption of O-mannose glycans within CHST1-expressing cells had a small but significant impact on Siglec-3 and -8 binding, demonstrating that this class of glycans can present sulfated Siglec ligands. We also investigated the ability of sulfated cis ligands to mask Siglec-3 and Siglec-7. For Siglec-7, cis ligands were again found to be mucin-type O-glycans. While N-glycans were the major sulfated trans ligands for Siglec-3, disruption of complex mucin-type O-glycans had the largest impact on Siglec-3 masking. Overall, this study enhances our knowledge of the types of sulfated glycans that can serve as Siglec ligands.



























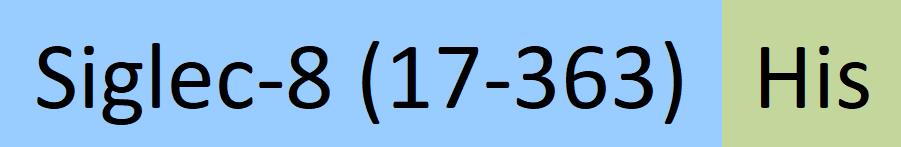
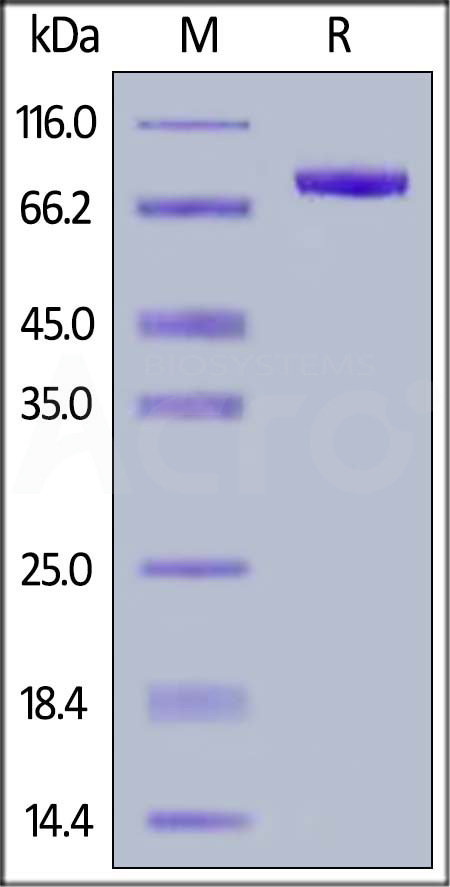
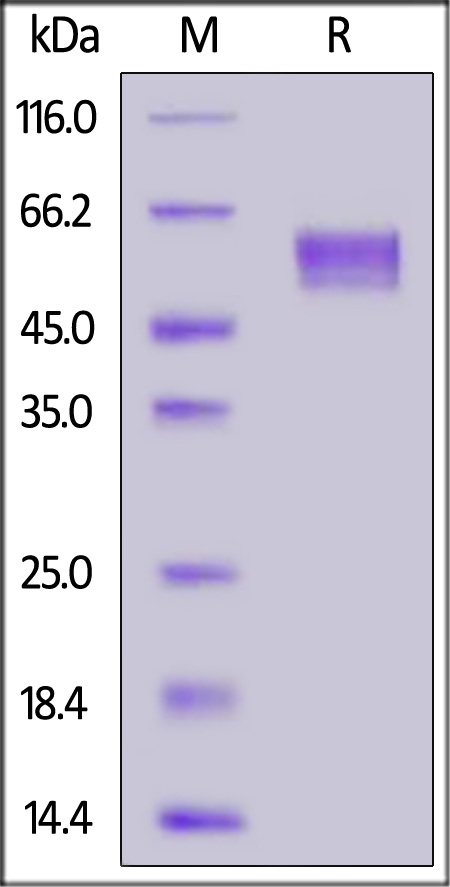
 Star Ribbon预染蛋白Marker蛋白质标记物是生物研究和药物开发的重要组成部分。无论是用于蛋白质电泳还是western blot,我们的预染色蛋白质标记物帮助您快速确定目标蛋白质的分子量或评估转移效率。Fc受体蛋白治疗性抗体的功效取决于Fab片段及其对目标抗原的结合活性,还取决于Fc片段及其与关键Fc受体的相互作用。因此,在抗体工程中候选物必须针对一系列受体进行测试。探索我们的重组Fc受体蛋白质的全面收藏!
Star Ribbon预染蛋白Marker蛋白质标记物是生物研究和药物开发的重要组成部分。无论是用于蛋白质电泳还是western blot,我们的预染色蛋白质标记物帮助您快速确定目标蛋白质的分子量或评估转移效率。Fc受体蛋白治疗性抗体的功效取决于Fab片段及其对目标抗原的结合活性,还取决于Fc片段及其与关键Fc受体的相互作用。因此,在抗体工程中候选物必须针对一系列受体进行测试。探索我们的重组Fc受体蛋白质的全面收藏!


























 膜杰作
膜杰作 Star Staining
Star Staining